"Bionic" Heart Patch Could Control Arrhythmia
Scientists at Harvard are developing a “bionic heart patch” that could be implanted and integrated into a patient’s heart tissue to monitor and regulate arrhythmias with greater precision than a pacemaker. Researchers say the device, which still is in early stages of development, could shed light on the efficacy of pharmaceutical treatments and correct pacing issues using smaller voltages.
During a heart attack, the cardiac muscle is starved for oxygen, and sections of cardiac tissue die or are scarred over in the aftermath of an attack. Once damaged, heart muscle usually does not regenerate on its own, and these weaknesses in the heart muscle can lead to a variety of complications, including valve problems, heart failure, or arrhythmias.
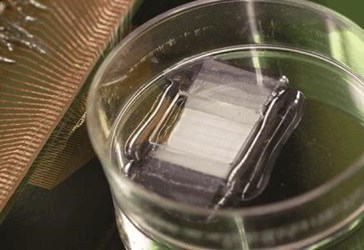
To offset these complications, researchers have developed a procedure called myocardial resection, in which damaged tissue is removed and replaced with a patch of healthy tissue, usually grown from a scaffold. A team at Harvard, led by Charles Lieber, is building a “smart” scaffold from silicon nanowires, which they claim could also monitor the condition of the heart and provide treatment as the heart heals, according to IEEE Spectrum.
“Our latest work shows for the first time a nanoelectronics-enabled scaffold with both size scale and mechanical properties on the same order of magnitude as conventional cardiac tissue scaffolds made of FDA-approved biomaterials,” said Lieber in an interview with IEEE Spectrum. Lieber added that his teams improved on previous work in the field by making a multi-layered scaffold both smaller and softer.
The smart patch, described in a study published in Nature Nanotechnology, combines sensing technology with mechanisms that could stimulate tissue, providing patients and doctors with real-time monitoring, as well as a means of correcting abnormal activities. Because the device would be inside the tissue, the patch would not have to use the strong voltages necessary with pacemakers.
Lieber commented that the research remains proof-of-concept, and his team is working on ways to improve the longevity of the device because silicone breaks down in the body over time, reported IEEE Spectrum. Lieber also suggested that his team’s previous research in injectable electronics used for brain monitoring may be compatible with the heart patch.
According to Lieber, the biggest impact of the research is its novel approach to regenerative medicine. “Rather than simply implanting an engineered patch built on passive scaffold, our work suggests it will be possible to surgically implant an innervated patch that would now be able to monitor and subtly adjust its performance,” said Lieber in a press release.
In March, researchers from Tel Aviv introduced what they’re calling a “cyborg heart patch” that will monitor the heart’s condition, regulate tissue conditions, and release anti-inflammatory drugs as needed. According to Haaretz, the team is looking into neurological applications for its research, developing patches for the brain and spinal cord.
