New Medical Device Reduces Vascular Scarring
By Chuck Seegert, Ph.D.
Delivering retinoid antioxidants to an artery that has undergone surgery with a newly developed biodegradable membrane has been shown to significantly reduce vascular scarring. Enhanced healing like this may lead to better long-term outcomes by preventing restenosis of vessels.
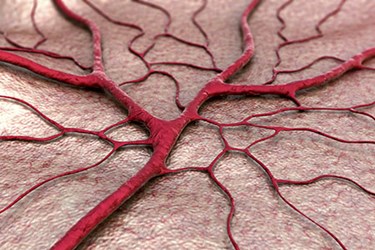
Arteries and other blood vessels that are involved in vascular interventions like grafting and stenting often undergo restenosis, or a closing off of the treated vessel, over time. This can lead to a second failure of the vessel, which puts the patient in a similar situation to where they were before his or her initial treatment. This scarring behavior is often the result of inflammation at the site of repair and oxidative stress that accompanies the healing cycle.
“Scar tissue will always form inside the blood vessel and, in many cases, eventually block blood flow,” said Guillermo Ameer, professor of biomedical engineering at Northwestern University’s McCormick School of Engineering, in a recent press release. “Then surgeons have to go back in, eliminate the obstruction, or put in a new graft or stent to restore blood flow. In the case of a prosthetic vascular graft used for bypass surgery, it will scar again and ultimately fail.”
In an effort to reduce the effects of oxidative stress in healing blood vessels, a newly developed antioxidant all-trans retinoic acid (atRA) was used at the site of surgery, according to a recent study published by Ameer’s team in American Journal of Physiology - Heart and Circulatory Physiology. The treatment with atRA has been shown to prevent intimal hyperplasia in healing vessels when administered orally, but this route led to side effects. To overcome this, the team used a local drug delivery method consisting of a polymer membrane that released atRA.
The membrane was wrapped around the outside of the vessel during surgery and then delivered atRA for about 2 weeks after surgery, according to the study. This led to a 50 percent decrease in restenosis (p=.001) in a rat model used by the team. The membranes also appeared to be well tolerated and biocompatible in the animal.
Damaged cells often orchestrate an inflammatory response, which then involves adjacent, normal cells. The presence of atRA mitigates this effect and keeps the cell signaling to a minimum, according to the press release.
“We’re putting something on the outside of the vessel that affects what happens inside the vessel,” Ameer said in the press release. “It seems counterintuitive, but scarring also involves cells that are normally present on the outside layer of the blood vessel.”
Recently, Ameer’s team disclosed another approach for vascular grafting that used a new biomaterial with inherent antioxidant properties.
