Asthma Sufferers Could Breathe Easier Thanks To New Wearable
Scientists at North Carolina State University (NCSU) have developed a health and environmental tracker (HET), a wearable system that aims to predict and potentially prevent asthma attacks by tracking lung function, activity rates, environmental factors, and other vital signs. The researchers have demonstrated proof of concept research and plan to further develop a smartphone app to accompany the system later this summer.
The Advanced Systems of Integrated Sensors and Technologies (ASSIST), which is centered at NCSU and funded by the National Science Foundation, works to develop health sensors that use nano-enabled energy harvesting techniques to power wearables without using batteries or external power sources. ASSIST director Veena Misra and her team of multidisciplinary scientists first introduced the idea of a HET project last year.
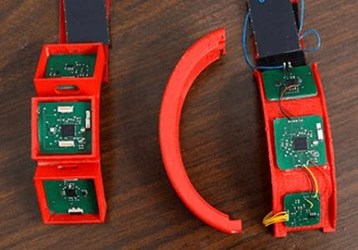
The system — described in a proof of concept study recently published in the IEEE Journal of Biomedical and Health Informatics — includes a multi-modal sensing platform integrated into a series of devices and software that compiles and analyzes data. A wristband tracks environmental asthma triggers, such as ozone and nitrogen dioxide, as well as the user’s activity and blood oxygen levels. A patch, which is worn on the chest, measures heart rate, respiratory rate, and wheezing in the lungs. Finally, an external spirometer, which is to be used several times a day, measures lung function and transmits data into the system.
According to Misra, comparable systems require hundreds of milliwatts of power that require substantial external power sources. ASSIST’s HET system, by comparison, can operate using sub-milliwatt levels of power, which could potentially be harvested from the body.
“This ultra-low power consumption is important because it gives the devices a long battery life, and will make them compatible with power-generated by the body — which is not a lot,” said Misra in a press release. “It enables a pathway to realize the ASSIST Center’s vision of wearable sensors powered by energy from the body in the near future.”
In the initial study, researchers tested the system on a limited number of human subjects and verified that the sensors worked and the software system accurately compiled data received. Future studies, said Misra, will attempt to drive power consumption even lower and develop a smartphone app that can analyze data and alert users to an oncoming asthma attack.
“This summer, we plan to begin testing HET in a controlled environment with subjects suffering from asthma and a control group, in order to identify which environmental and physiological variables are effective at predicting asthma attacks,” said Misra.
James Dieffenderfer, lead author of the study and a PhD student on Misra’s team, commented that preventing an asthma attack could one day “be as simple as going indoors or taking a break from an exercise routine.”
The CDC estimates 18.7 million adults and seven million children suffer from asthma in the United States, a condition that costs, on average, $56 billion in annual healthcare costs and loss of productivity.
Philips recently introduced a wearable capable of diagnosing pneumonia, and a wearable under development at Michigan State University uses wireless radio signals to track patients with diabetes, athsma, or even depression. A recent report from Tractica projects that the global healthcare wearables market will reach $17.8 billion per year by 2021.
