Case Of Mistaken Identity: A Medical Device Company's 22-Year Classification War With FDA
By Tracey B. Kirsch, president, Electromedical Products International, Inc.
When dealing with a government agency like the Food and Drug Administration (FDA), the most cynical among us anticipate lag times between communications, hearing delays, back-and-forth between legal teams, and lost, missing, and just plain misunderstood information. But in the confrontation between the FDA and makers of cranial electrotherapy stimulation devices (CES), no one expected a legal battle that would drag on for 22 years, nearly crippling a company and giving an entire industry a black eye.
Electromedical Products International (EPI) has been the lead player in a protracted dispute with the FDA regarding its medical device classification of CES devices, which only this past June was resolved when the agency promised to reverse a long-standing decision. The controversy concerned what we believed was a misclassification of our microcurrent devices that treat pain, anxiety, depression, and insomnia. The agency classified the CES indications into a Class III, which put them in the same category as tightly regulated high-risk medical devices such as pacemakers and heart valves.
The FDA is charged with categorizing medical devices based on the risks associated with the device. The agency’s website defines the classifications as follows:
- Class I devices are deemed to be low-risk and are therefore subject to the least regulatory control. For example, dental floss is classified as Class I device.
- Class II devices are higher-risk devices than Class I and require greater regulatory control to provide reasonable assurance of the device’s safety and effectiveness. For example, condoms are classified as Class II devices.
- Class III devices are generally the highest-risk devices and are therefore subject to the highest level of regulatory control. Class III devices must typically be approved by FDA before they are marketed. For example, replacement heart valves are classified as Class III devices.
Back in 1976, when the FDA first began to regulate medical devices, there were about 25 categories that were literally dumped into Class III, because the FDA did not believe that sufficient information existed to ensure the devices were reasonably safe and effective. The law required the FDA to review and appropriately recategorize those temporarily placed in Class III within 36 months. However, 33 years later, the Government Accountability Office (GAO) officially reported on the FDA’s failure to reclassify these devices.
Unfortunately, cranial electrotherapy stimulation devices were among those that fell prey to the agency’s dump-and-run handling of this assignment. This classification of CES devices resulted in confusion about their safety and effectiveness by medical practitioners, the insurance industry, and even the general public, who assumed that CES was a potentially high-risk device when it was nothing of the sort. Thus began the misrepresentation of CES devices, an extremely safe and effective alternative to medication in the treatment of anxiety, depression, and insomnia.
Keeping The Business Going During A Protracted FDA Battle
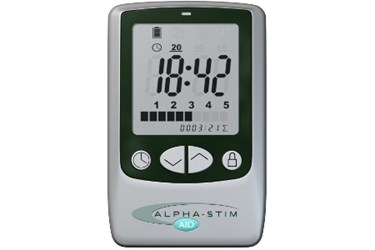
We were lucky in the sense that Alpha-Stim, our product, has two clearances: one for pain control and one for use as a CES device. While we challenged the CES classification, we focused our attention on expanding our market for treating pain. That helped generate cash flow and kept us in front of medical professionals, both of which were critical to our survival.
During this time, we continued investing in the technology, taking advantage of new advances and making sure our devices reflected the best and latest tech possible. In addition, during this period, a number of interested individuals approached us about conducting research on Alpha-Stim. This was important research in the field, being conducted by individuals who were curious — rather than by paid consultants — and offered further evidence of the medical benefits of CES and Alpha-Stim.
We also expanded into markets outside of the United States, but even here at home, the effects of the FDA classification were felt, as some countries take their regulatory cues from the U.S.
The events of September 11, 2001, prompted our desire to help military service members and veterans who defended our way of life. The best way we could contribute to America’s efforts was to help relieve the pain and stress of those who fought and are fighting for our country. It took 18 months to get on the Federal Supply Schedule (FSS) — not an easy process for a small company — but our first inclusion in the FSS was on April 15, 2005. We have been serving our veterans and service members ever since, and all of our employees take a great deal of pride in the fact that today they are one of our biggest accounts.
A Case of Mistaken Identity?
While the misclassification was difficult enough, what followed over the next two decades nearly shut down the CES industry. The FDA required CES devices to go through the full premarket approval (PMA) process, which is a complicated, time-consuming, and expensive undertaking. In spite of repeated reviews, the process was never completed by the FDA and, due perhaps to the fact that FDA reviewers had no personal experience with CES, the devices repeatedly ended up back in Class III, requiring a PMA.
Over the ensuing years, there was considerable back-and-forth between EPI and the FDA, much of it repeated, frustrating, hurry-up-and-wait experiences.
As a small healthcare business owner, it is hard to be so at odds with an agency we all personally felt provided some much-needed oversight in the medical industry. But the way the agency operated demonstrated a clear lack of consistent standards in reviewing medical devices, and an arbitrary application of its own definitions and standards for them.
Finally, in June 2014, the FDA issued an intent to reclassify CES devices, which all involved parties welcomed. Finally, closure could come to an extremely costly, time-consuming chapter in our business. It remains to be seen when that reclassification will actually take place.
6 Tips For Handling An FDA Culture Clash
As I look ahead to the future, I’m excited about where we are as a company, and about the potential for our industry as a whole. I anticipate that the down-classification of CES devices will result in our obtaining an insurance code for CES, which opens new doors for us and benefits health care providers and patients.
We plan to explore new indications for Alpha-Stim, and work on obtaining clearance for use in other therapeutic applications.
Having been through what we have with the FDA, I believe we are more confident and better prepared to prove the value of CES as a therapy, and focus on growing our business and taking advantage of opportunities as they open to us.
In conclusion, I would like to share some of our learnings with other medical device companies that are dealing with an FDA culture clash:
- Know your own business. You need to be able to defend yourself in a logical, persuasive, and above all, truthful manner.
- Know your elected officials. These folks work for you! In our experience, the FDA doesn’t much like getting letters from Congressional representatives, and tend to take notice when it happens.
- Know the law. Understand your rights. No one is perfect, no agency is perfect, and mistakes can be made. It is up to you to be able to defend yourself against those mistakes.
- There is real power in grassroots action. We got people to write to the docket. The public has the right to comment, and it becomes part of the record.
- Get yourself a good FDA law attorney. Ours was invaluable, providing support that only an expert in this arena could.
- It is OK to respectfully disagree. The key here is “respectfully.” And if you disagree, you better be prepared to back it up.
About The Author
 Tracey B. Kirsch is president of Electromedical Products International, Inc. (EPI), where she oversees all financial matters, human resources, regulatory affairs, and daily operations. She was instrumental in gaining regulatory approval for the company’s products in many countries including Europe (CE Mark), Australia, Canada, China, and various countries in South America, Africa, and the Middle East. In 2005, she negotiated a Federal Supply Schedule contract with the U.S. government for use of Alpha-Stim within the Department of Defense and Veteran’s Affairs Medical Centers.
Tracey B. Kirsch is president of Electromedical Products International, Inc. (EPI), where she oversees all financial matters, human resources, regulatory affairs, and daily operations. She was instrumental in gaining regulatory approval for the company’s products in many countries including Europe (CE Mark), Australia, Canada, China, and various countries in South America, Africa, and the Middle East. In 2005, she negotiated a Federal Supply Schedule contract with the U.S. government for use of Alpha-Stim within the Department of Defense and Veteran’s Affairs Medical Centers.
Kirsch joined the five-member board of directors for the not-for-profit organization American Institute of Stress (stress.org) in 2012. She oversees all business and accounting activities for AIS and helps plan and execute the institute’s business.
She has taught programs on Agency Policy and Procedures, Clients’ Rights, Federal Regulations Survey and Follow-up, among others. In January 2015, she and her husband / business partner Dr. Daniel L. Kirsch authored a chapter covering the U.S. Food and Drug Administration’s medical device regulatory processes for the book Bioelectromagnetic and Subtle Energy Medicine, Second Edition (CRC Press).
