How Implant Size And Shape Affect Immune Response
Massachusetts Institute of Technology (MIT) scientists have determined that certain sizes and shapes of implantable devices are tolerated better by the body. By optimizing implant design, the researchers say device developers can reduce the likelihood of a foreign body reaction (FBR).
Contrary to what one might think, larger implants can fare better than smaller, said researchers in an article published by MIT News. In a series of experiments using a variety of different materials, researchers reported that they achieved the best results with spherical shapes 1.5 mm or larger.
The team made its discovery while developing an implantable device that mimics the function of the pancreas by delivering pancreatic islet cells to replace the nonfunctional cells in Type 1 diabetics. If successful, the implant could eliminate the need for insulin injections, but first the cells have to be delivered in a device that will not trigger an immune response and scar over.
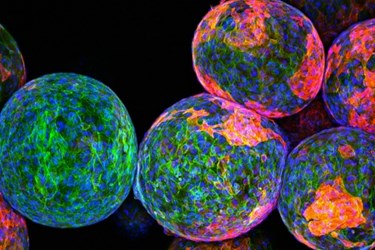
In a study published in Nature Materials, researchers implanted devices of two different sizes — 0.5 mm and 1.5 mm — in the stomachs of diabetic mice. They discovered the smaller spheres scarred over and were rendered inactive after one month, but the larger spheres continued to function after six months.
The original device was designed using alginate, but researchers tried other materials such as ceramics, glass, metals, and plastics. Regardless of the material used, the larger spheres performed better and “significantly abrogated FBRs and fibrosis when compared to smaller spheres,” said study authors.
“When we first got this data, it was counterintuitive,” said Daniel Anderson, an MIT professor of chemical engineering and senior author of the study. “There was reason to think when you have these little small beads they would elicit less of a response, but it just wasn’t the case.”
“What it’s made of is still an important piece of the puzzle, but it turns out if you really want to have the least amount of scar tissue you need to pick the right size and shape,” said Anderson.
Though the team intends to apply this new insight to the design of an artificial pancreas, they say the new understanding will help other device developers refine their designs.
Related, researchers at Cambridge last year released findings from a study that found the stiffness of an implantable device can trigger an FBR, and they concluded that coating a device in a material matching the texture of surrounding tissue could greatly reduce the chance the device would be rejected.In an opinion piece published alongside the MIT study, Ruud Bank, a professor at the University Medical Center Groningen, commented, “Because of an aging population, there is an increasing demand for tissue implants and implanted delivery systems, which calls for increased efforts to better understand the FBR.”
Image credit: Andrew Bader, Omid Veiseh, Arturo Vegas, Anderson/Langer Laboratory, Koch Institute at MIT
