Microfluidic Device Shows Promise As Ventilator Alternative
A new microfluidic gas exchange device could represent a safer alternative to mechanical lung ventilation and extracorporeal membrane oxygenation (ECMO) systems. Because the new technology more closely mimics the environment of the lung, researchers believe it would provide a reduced risk of blood clotting.
Patients unable to spontaneously draw breath because of disease or injury are often put on a ventilator that assists oxygen/carbon dioxide exchange by pushing oxygen into the lungs. Studies show that mechanical ventilation with positive pressure increases a patient’s risk of developing pneumonia, tissue damage, injuries to the airway, and lung remodeling. Experts argue that forcing air into damaged lungs gives them little opportunity to heal.
Jeff Borenstein, a bioengineer at the Charles Stark Draper Laboratory (Draper), told MIT Technology Review that putting a patient on mechanical ventilation is like making a person “exercise a broken arm.”
High-risk patients unsuitable for ventilators — such as prematurely born infants — are considered for an alternative technology, ECMO, a process that draws blood out of the body and filters it through a machine that swaps out carbon dioxide for oxygen, and then returns the blood to the body. Though these systems are often a patient’s only hope for survival, they are highly complex and require an experienced technician to monitor closely for potential problems. One of the most common risks associated with ECMO is blood clotting, and patients undergoing ECMO treatments are put on high doses of blood thinners, which carry additional risks.
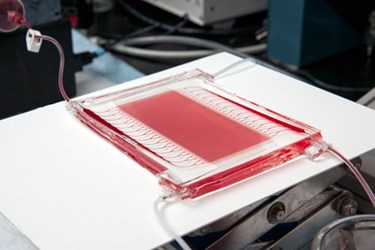
Borenstein told MIT Technology Review that existing ECMO systems use a bundle of porous fibers, a foreign environment not suitable for high volumes of blood flow. As an alternative, Borenstein and his team at Draper have designed a multi-fluidic device that allows blood to flow through layers of biocompatible plastic molded into a “three-dimensional branching structure,” similar to lung vessels branching into capillaries.
Until now, multi-fluidics have mostly been small in scale, used for diagnostics and lab-on-a-chip technology for new drug investigations, but Borenstein believes that the technology is capable of larger scale undertakings.
In a Draper press release, Borenstein said “Microfluidic technologies have shown promise for small-scale lab-on-a-chip applications, but the Draper projects show for the first time how microfluidic devices can be scaled for high blood flows required for acute interventions and chronic support.”
The Draper team’s studies of the device using cow blood demonstrated a flow rate of 100 milliliters per minute, which the team is working to speed up to multiple liters per minute. The researchers believe that, with further improvements, the technology could be appropriately scaled for humans.
Phillip Camp, a cardiothoracic surgeon at Bringham and Women’s Hospsital in Boston, told MIT Technology Review that such a device would be “revolutionary” in respiratory care. According to Camp, Draper’s device is much simpler and more efficient that existing ECMO machines, and because of its lower blood clot risk, it would be much safer for long-term use, or for patients experiencing flare-ups of chronic conditions, such as chronic obstructive pulmonary disease (COPD).
