New Hybrid Heart Valve Design Combines Metal, Engineered Tissue
Scientists at the University of California, Irvine (UCI) have developed a heart valve replacement made from a combination of metal and engineered tissue. Because the new hybrid valve is both patient-specific and durable, researchers believe it could overcome complications caused by existing valve replacement options.
A recent study, conducted at Mount Sinai Hospital, compared the survival and long-term outcomes of patients between the ages of 50 and 69 who had received either mechanical aortic valve replacements or animal-harvested bioprosthetic valves.. While researchers found no significant long-term differences in patient survival, they discovered that bioprosthetic valves were more likely to require reoperation within 10 to 15 years, and mechanical valves were more likely to cause major bleeding and clotting, and to require a long-term regimen of anti-coagulants.
Newer, tissue-engineered valves, cultured from a patient’s own cells on a biodegradable scaffold, have a tendency to shrink after the scaffolding is absorbed into the body, causing the valve to malfunction, stated UCI scientists in a recent press release.
In an effort to incorporate the advantages of all three valve replacement options and to offset their respective disadvantages, researchers at UCI developed the hybrid valve, made from a nickel-and-titanium alloy (nitinol) and engineered tissue.
“For our research, we decided to use a non-degradable scaffold that stays within the valve to provide the support it needs without interfering with its normal function,” said Arash Kheradvar, a UCI scientist who developed the valve with fellow UCI researcher S. Hamed Alavi.
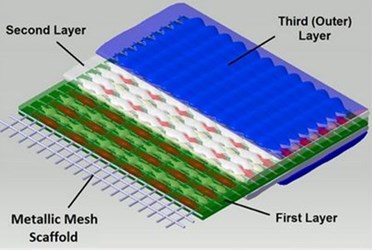
In a study published in The Annals of Thoracic Surgery, the researchers describe the valve as a “trileaflet Nitinol mesh scaffold” enclosed in a “three-dimensional cell culture with smooth muscle and fibroblast/myofibroblast cells” that are covered by a endothelial cell layer. The entire construction process can take anywhere from three to eight weeks.
Kheradvar and Alavi tested their hybrid valve with a heart flow simulator and found that the hybrid valves “open and close robustly under physiologic flow conditions with an effective orifice area of 75 percent.”
In the press release, the researchers stated that the hybrid valve likely would regenerate inside the body and become a permanent “living” part of the patient’s heart structure.
“We believe this new hybrid technology will significantly improve a patient’s quality of life by eliminating the need for lifelong medications and without compromising the durability of the valve. This is particularly beneficial for younger patients who are in need of a valve replacement,” said Alavi.
The researchers plan to pursue the next stage of clinical testing with the hybrid heart valve, and they anticipate that it could be ready for use in patients within five to 10 years.
The University of Maryland Medical Center estimates that more than 5 million Americans are diagnosed with heart valve disease each year. While the disease can occur in any combination of the four heart valves, the aortic and mitral valves are the most commonly affected.
