Blocking Certain Immune Cells Could Prevent Scar Tissue From Forming On Implants
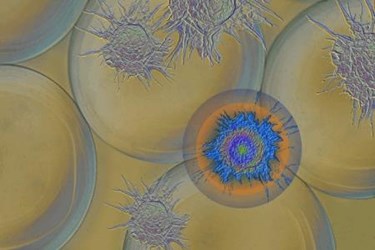
New research has shown that, by selectively blocking certain immune cells, scientists may be able to prevent the formation of scar tissue on implanted medical devices, which could substantially improve their biocompatibility and extend their functional use. The technology — which was tested on alginate, plastic, and ceramic implants — was developed by a team of scientists at Massachusetts Institute of Technology (MIT) working on an artificial pancreas implant for patients with type 1 diabetes.
One of the greatest challenges of engineering implants is designing a device large enough to be effective, but small enough to avoid rejection by the body’s immune system, which often results in the formation of scar tissue that can be especially damaging to electrical systems. Common strategies for surmounting these obstacles include advances in wireless technology, biocompatible materials, and anti-inflammatory or immune-suppressing drugs.
The MIT Scientists, led by Daniel Anderson, have taken a different approach to improving biocompability, one that MIT scientist Robert Langer told MIT News is among the first studies to examine the “fundamentals” of immune responses to biomaterials. By examining the earliest signs of scar tissue formation (fibrosis), scientists were able to isolate a specific molecule that triggered the process, and were able to block it without significantly compromising the immune system.
CSF1R is a molecule that appears when monocytes differentiate into mature macrophages, a process that triggers fibrosis. In a study published in Nature Materials, the researchers describe their isolation of CSF1R by systematically blocking several immune system components in mice. By blocking cell receptors for this molecule, the researchers were able to prevent the formation of scar tissue on several different biomaterials, including ceramic, a plastic called polystyrene, and alginate.
“We show that you preserve many other important immune functions, including wound healing and phagocytosis, but you lose this fibrotic cascade,” said Joshua Doloff, a post-doctoral researcher working in Anderson’s lab. “We’re preventing the macrophages from toggling into an activated warning state where they sound the alarm for this massive immune response to show up.”
Doloff added that the potential drug would be “generalizable” for many types of biomaterials and for many different applications, and would potentially be more effective than broader-purposed immunosuppressive drugs that could block essential functions of the immune system.
The research grew out of the efforts of Anderson’s team to build a “pancreas in a capsule,” an implant of insulin-producing islet cells created using stem cells. Currently, the researchers are using a shell of alginate to hold and protect the islet cells, but have found that even this biomaterial is prone to fibrosis.
“I am very impressed with this paper, particularly with the identification of CSF1R as a target,” says Gordon Weir, co-head of the Joslin Diabetes Center’s division for regenerative biology. Future research, said Weir, should investigate how long the CSF1 would need to be suppressed and what long-term effects this could have on the body’s immune system.
Aaron Kowalski, chief mission officer for the Juvenile Diabetes Research Foundation (JDRF), which provided partial funding for the research, commented that the project is an “incredible step forward” in JDRF’s mission.
