DARPA Begins Funding "Electroceutical" Research
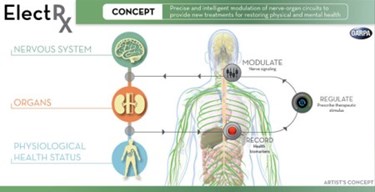
The Defense Advanced Research Projects Agency (DARPA) has launched the first seven research projects of its Electrical Prescriptions (ElectRx) program, which seeks to reframe the approach to modern medicine and chronic illness. By studying and treating the body as a system of electrical circuits, scientists may be able to develop more effective methods for managing diabetes, rheumatoid arthritis, and traumatic battlefield injuries and psychological conditions.
The $78.9 million research project announced last year aims to develop nanoscale devices that can be implanted or even injected into the body to modulate the peripheral nervous system’s response to sickness or trauma. DARPA’s project manager David Weber said in a statement that the tiny devices would “continually assess conditions and provide stimulus patterns tailored to help maintain healthy organ function, helping patients get healthy and stay healthy using their body’s own systems.”
According to Forbes, similar research is already underway developing treatments for Alzheimer’s, but the key to the future success of the project will be effectively downsizing the devices, which currently are the size of a deck of cards.
Since President Obama announced the program, DARPA has been collecting proposals for research projects, and this week the agency announced the first seven teams set to receive a portion of the allotted funding, provided by the White House’s BRAIN Initiative.
Since the project is still in its early days, most of the initial projects receiving grants are exploratory and geared toward understanding nerve pathways and the most effective means of providing stimulation, whether it’s pulses of light, magnetic fields, or sound waves.
For example, Circuit Therapeutics, a start-up based in California, will be investigating optogenetic methods for treating neuropathic pain, and a team at Columbia University will be looking at the impact of non-invasive targeted ultrasound on neuromodulation. A Johns Hopkins team hopes to make a connection between the sacral nerve and inflammatory bowel disease, and researchers at Massachusetts Institute of Technology (MIT) will work to refine their research using magnetic nanoparticles to target the adrenal gland.
Purdue University, the University of Texas, and the Florey Institute of Neuroscience in Australia are all looking into the vagus nerve, a target that a recent IEEE Spectrum article called a “back door for brain hacking.” According to the article, early clinical results indicate that “electroceuticals” have fewer — if any — side effects and would be cost-comparable to their pharmaceutical counterparts.
David Weber hopes that future projects will move toward devices that can detect biomarkers at the onset of disease or trauma and trigger a neural response, or detect low blood sugar and send messages to the pancreas. Essentially, these devices would help the body to heal itself both at home and on the battlefield.
“Using the peripheral nervous system as a medium for delivering therapy is a largely new territory and it’s rich with potential to manage many of the conditions that impact the readiness of our military and, more generally, the health of the nation,” said Weber in the statement. “It will be an exciting path forward.”
