How Medical Device Developers Can Create Better Dental Medtech
By Jon Caulfield, DDS, PC
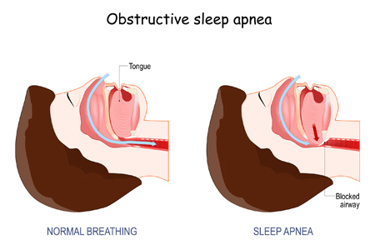
Ninety-eight percent of patients with obstructive sleep apnea (OSA) syndrome have abnormal anatomical features of the soft tissues and/or the structures of the maxillomandibular skeleton, which cause a disproportionate anatomy of the airway. Beyond the obvious issues with sleep and breathing, this anatomical deficiency that leads to OSA also contributes to high blood pressure/hypertension, heart failure, stroke, coronary artery disease, countless other comorbidities, and life-threatening illnesses in patients.
Today, many physicians are aware of and utilize continuous positive airway pressure (CPAP) and other supportive treatments, but these fail to address the root cause of OSA and can even make matters worse when these therapies adversely affect anatomical features and soft tissues.
Some progress has been made in recent years to create innovative medical technology and devices that focus exclusively on the tongue, thus addressing awareness of a potential root cause of OSA and other sleep-related disorders. However, there are still gray areas for medical device creators when it comes to how next-generation technology can solve anatomical deficiencies from the moment a device or technology is created.
Consider The Evolution Of The Tongue And Its Role In OSA
Generations ago, the tongue and its positioning in the mouth were quite different than it is today. Archaeological findings have revealed that just a few centuries in the past, human jaw growth and development were maximized, allowing for 32 teeth to fully occupy the intraoral space. This was mostly due to tongue positioning and functioning with nasal breathing and dietary habits.
In the years since, we have seen a dramatic decrease in jaw growth and development, as well as the increase in tooth crowding, removal, and insufficient tongue space, which has been attributed to industrialization and westernization, including bottle feeding, inadequate breast feeding, soft diets, and allergy development, with overall physical and physiologic changes to the everyday functions of breathing, eating, and sleeping. Of course, with the oral cavity being innately grown and developed based on the function and form of the tongue, these evolutionary changes make sense. But if the oral cavity is not grown correctly, underdevelopment results, and there is no way for the tongue to move forward or laterally, which results in it being restricted and forced back into the airway. This is where medical device developers must look.
Current solutions like CPAP and other modalities do not address this underdevelopment and insufficiency. To create oral devices that get to the root cause of OSA and solve breathing issues permanently, medical device creators would benefit from additional education on how the human tongue and jaw have evolved so they can develop innovations that address these changes, rather than cover them up with temporary fixes.
By encouraging further education on maxillary development and increasing intraoral tongue space for medical device developers, anatomical deficiencies can be improved and overcome to allow for corrective breathing and airway flow dynamics. Additional therapies used in conjunction with this anatomical improvement can also strengthen the tongue and associated soft tissues while restoring physiological nasal breathing, allowing patients to have better daytime and night-time respiration.
Consider The Role Of The Nose
Nasal breathing is key to proper growth and development of the airway as well as filtering, sterilizing, warming, and humidifying the incoming air while preparing it for delivery to the lungs for respiration while awake and sleeping. Nasal valve stenosis, or collapse, is a major issue that can cause blockage of the airway and difficulty breathing. It is most often treated with surgery or managed physically with a nasal valve dilator.
While mute dilators can be inserted, and they offer different sizes with several inter-nasal distances as well as have an adjustable dilation system to adapt to each nasal passage individually, options for repair and prevention of nasal valve collapse need to be developed to allow better nasal breathing and function for sleeping patients. Medical device developers should focus on adjusting such successful devices to not only establish breathing but also maintain the system against collapse.
Consider Internal Obstructions
Nasal obstruction is usually caused by either swelling of the nasal tissue or an anatomical blockage, which can lead to sleep disorders, snoring, and OSA. Anatomical factors such as a deviated nasal septum, enlarged turbinates, nasal polyps, enlarged adenoids, or nasal tumors can contribute to nasal obstruction and reduce the airflow in and out of one or both nasal passages. Tonsils can also become so swollen that they can block off the back of the throat and the airway. Swollen tonsils are a common cause of OSA and, typically, surgical removal is required (American Sleep Apnea Association). Excessive and flaccid palatal tissue can also be a source of obstruction for many patients suffering from OSA. The tongue can exacerbate this condition if it is not properly positioned forward and away from the palate. Palate surgery, such as uvulopalatopharyngoplasty (UPPP), aims to enlarge the area around the tonsils and the soft palate by removing excessive tissue and tightening flaccid tissues; it has been used in the past, but it is often not as effective in treating OSA. Lasers and other modalities have also been used to tighten the tissues and aid in the treatment of OSA as of late, with some success.
More advances are needed in treating these obstructions, and a focus on developing medical technologies to assist in this endeavor would be highly valuable in managing and treating patients with OSA. Though the current tools available do provide some relief, most solutions are not intended to be used long-term. Beyond the need to hygienically maintain the devices and the less than 24-hour recommended wear time, most products available involve inserting foreign material into the nasal cavity to stabilize the passage. If developers could create devices that did not further obstruct airways and that could be used consistently, and, ultimately, modify the source of the problem as opposed to simply managing the symptoms, patients would have better outcomes time and time again.
Conclusion
Our evolving anatomy plays a critical role in the underlying causes of sleep-related breathing disorders and obstructive sleep apnea. Unfortunately, not enough attention has been given to the reasons why the disease has been allowed to appear and propagate. This is where medical technologies can assist physicians and dentists in preventing these issues in children before they become lifelong issues or having to correct or improve these issues in adults. Doing so could be the key to achieving resolution and elimination of the disease itself.
A full-spectrum system to support anatomical, physiological, and biological improvement is needed to address this critical health issue and dramatically improve overall health while reducing associated diseases and comorbidities. The anatomical improvement is one that can be influenced and addressed immediately, and it can assist in physiological and biological improvements to arrest and reverse the growing population of patients suffering from obstructive sleep apnea. By allowing the body to function the way it was designed and meant to function, with proper form and anatomy, many of the interrelated interactions within the human system can correctly function as well.
The reality is that ending OSA for good lies more in the hands of medtech developers, and not nearly as much in doctors and dentists. If new medical technologies can be developed to address the anatomical form and help to enhance the physiological functions of breathing and sleeping, a marked improvement can be seen in many OSA patients’ overall health and lifestyles.
 About The Author:
About The Author:
Jon Caulfield, DDS, PC, is an independent dentist at Epic Dentistry in Littleton, Colorado, and leverages the Vivos Method to address dental tissue anomalies that are known to be associated with OSA and other debilitating health conditions.
