4 Key Takeaways For Combination Products As We Move Into 2023
By Fran DeGrazio, Strategic Parenteral Solutions LLC
The world of combination products has been evolving ever since the FDA final rule on cGMP practice requirements for combination products was issued on Jan. 22, 2013. It was followed by the FDA’s final companion guidance on the same subject that was released in January 2017. As the use of combination products in industry and around the globe continues to grow, corresponding challenges in this space also grow.
The FDA defines a combination product as a product composed of any combination of a drug and a device; a biological product and a device; a drug and a biological product; or a drug, device, and a biological product.
To stay abreast of this dynamic segment of the industry and its associated regulatory expectations, meetings such as the AFDO/RAPS Combination Product Summit have been held. (AFDO is the Association of Food and Drug Officials, and RAPS is the Regulatory Affairs Professionals Society.) Historically, this meeting had been coordinated by Xavier Health. This year, for the first time, the AFDO/RAPS Healthcare Products Collaborative coordinated the summit, and it was again co-sponsored by the FDA. The planning of this meeting involves industry leaders along with representatives of the FDA’s Office of Combination Products (OCP). I delve into the summit’s four key takeaways below.
1. Recent & Upcoming Activities Shared By The Office of Combination Products
The main summit session opened with an overview from FDA representatives of the Office of Combination Products. Key takeaways related to the process of Request for Designation (RFD). In the past year, the vast majority of submissions for this process were returned to the sponsors because not enough of the appropriate information had been shared with the FDA. So, applicants benefit if they have a better understanding of the detail needed to be submitted as part of the request.
OCP continues to work to support the industry, not only in working to assure inter-center consultation occurs but also to provide guidance to the industry, when possible. There were two guidances finalized and released in 2022 relating to combination products. These were:
- Principles of Premarket Pathways for Combination Products (January 2022)
- Alternative or Streamlined Mechanisms for complying with CGMP requirements for Combination Products (September 2022)
In addition, there are seven pending guidance documents that should be released in final or draft formats (release dates TBD). These are:
- Human Factors of Combination Products (final)
- Essential Performance Requirements (EPRs) Established Condition & Combination Products (draft)
- Technical Considerations For Demonstrating Reliability Of Emergency-Use Injectors (final)
- Combined Use/Cross-Labeled Combination Products (draft)
- Post-Market Changes To Combination Products (draft)
- Guidance On Unique Device Identifiers & Combination Products (draft)
- Labeling Considerations For Insulin Pumps (draft)
2. We’re Moving Toward Global Regulatory Alignment
There was also industry recognition that there are challenges with harmonization from a global regulatory perspective. The industry, for instance, is trying to get a better understanding of the definition of a significant change under the European Medical Device Directive (EU MDR). It was acknowledged that leveraging risk management and moving past semantics will help with alignment. The use of Association for the Advancement of Medical Instrumentation (AAMI), International Organization for Standardization (ISO), and other standards organizations will help to slowly bring more consistency from a global perspective.
An example of one of these is American Society for Testing and Materials: ASTM 55 -International Combination Products Terminology Standard. This document is currently under final review and approval within several regulatory agencies. When this is finalized, there should be alignment among FDA, European Medicines Agency (EMA), and Health Canada at a minimum.
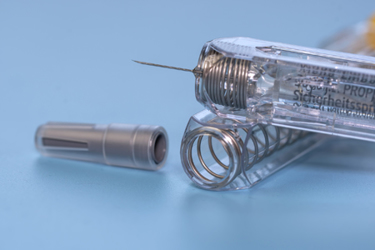
3. The Transition To ISO’s Newest Standard On Needle-Based Injection Systems Ends In July 2023
One of the challenges in the industry has been the publication of various guidances and standards through the years. These are needed to provide direction; however, it is a challenge, at times, to be aware of all of these from a global perspective. One of the key newly released documents is ISO 11608-1:2022 Needle-based injection systems for medical use. This document provides requirements for needle-based injection systems for single patient use intended to deliver a discrete volume of a drug. The transition period to move to this recently released standard ends on July 9, 2023.
The entire document should be reviewed, but some of the key areas that differ vs. prior versions include adding the term and action of identifying primary functions (PF), clarifying guidance around the need for combined preconditioning testing, and the addition of an entire new section (-6) to address on-body delivery systems. This standard continues to reinforce and strengthen design control, risk management, and human factors.
4. Addressing Digital Health Challenges
Several sessions addressed various aspects of digital health or connected systems. It is clear this continues to be a developing area for the industry (readers may be aware that the FDA’s Center for Devices and Radiological Health launched a Digital Health Center of Excellence in September of 2020). Important factors that cut across any type of product in these categories are the fact that the regulatory pathway must be clearly understood. This means that early engagement with the regulatory agency is a must.
Additionally, useability and human factors studies will be key up front and during development to assure an understanding of the user groups and user environment.
A strong quality system designed specifically with digital health technologies in mind must be instituted. A series of unique considerations must be incorporated, such as deployment of an application in the app store, understanding and communicating security vulnerabilities, and informing stakeholders about how to handle decommissioning, as examples.
There was discussion around Software as a Medical Device (SaMD) vs. the use of software that is not considered a medical device. In its simplest terms, software functions that analyze or interpret data are subject to regulatory oversight as SaMD in the U.S. If the software, instead, is intended to transfer, store, convert format, or display data it is considered a medical device data system (MDDS). In this case, the software is isolated from the device function. In any case, it is imperative that the risk profile of each component of the system be considered for the cascading impact at the individual system and ecosystem levels.
About The Author:
 Fran DeGrazio is president & principal consultant at Strategic Parenteral Solutions LLC currently a Kymanox Executive Advisor. She has more than 35 years of experience in the pharmaceutical packaging and delivery industry with extensive expertise in sterile drug product systems, including vial container closure systems and prefillable systems for combination products. Prior to her consultant role, she held numerous technical roles at West Pharmaceutical Services, including R&D, quality & regulatory, technical customer support, analytical laboratories and scientific affairs, and most recently as chief scientific officer. She is the recipient of the PDA Packaging Science Award for 2021, Philadelphia Business Journal 2018 Healthcare Innovators of the Greater Philadelphia Region Award, and the Healthcare Businesswoman’s Association Luminary Award for West in 2017.
Fran DeGrazio is president & principal consultant at Strategic Parenteral Solutions LLC currently a Kymanox Executive Advisor. She has more than 35 years of experience in the pharmaceutical packaging and delivery industry with extensive expertise in sterile drug product systems, including vial container closure systems and prefillable systems for combination products. Prior to her consultant role, she held numerous technical roles at West Pharmaceutical Services, including R&D, quality & regulatory, technical customer support, analytical laboratories and scientific affairs, and most recently as chief scientific officer. She is the recipient of the PDA Packaging Science Award for 2021, Philadelphia Business Journal 2018 Healthcare Innovators of the Greater Philadelphia Region Award, and the Healthcare Businesswoman’s Association Luminary Award for West in 2017.
