Making The Case For AI-Enabled Coronary CT Angiograms
By James K. Min, MD, FACC, FESC, MSCCT
For more than 50 years, cardiovascular disease (CVD) has remained the leading cause of death in the United States, claiming the lives of more than 650,000 people annually. While heart disease mortality has experienced a steady decline in recent decades, our progress has now stalled. The latest science demonstrates that we are stagnating in our fight against heart disease, with rates of heart attacks now increasing in high-income countries. Unfortunately, we will soon witness a startling increase of this already tragic public health epidemic.
Underlying this urgent need is the disproportionate toll cardiovascular disease continues to exact on minority populations. Black patients are two times as likely to die from heart disease than white patients. The causes of these disparities are multidimensional but directly relate to social determinants of health, including food security, education, transportation, and housing. In turn, minority populations confront far more barriers to CVD diagnosis and access to care, receive lower-quality treatment, and experience worse health outcomes.
To support heart disease evaluation for all patients and change these deep divides, we must re-evaluate our population-based approaches to heart disease evaluation and embrace proactive precision heart care methods that meet patients where they are.
Personalizing Cardiovascular Care: From Indirect To Direct Evaluation Of Heart Disease
Historically, approaches to support patients with suspected heart disease have been restricted to indirect markers of disease rather than assessing an individual’s primary atherosclerotic plaque itself. For example, in asymptomatic individuals, the conventional method to assess heart attack risk is to evaluate a patient’s risk factors (e.g., cholesterol) as a surrogate to heart disease, a practice successful at discriminating risk of populations of people, but one that fails to precisely pinpoint individuals with significant heart disease. Similarly, for symptomatic patients presenting with chest pain or shortness of breath who are suspected to have heart disease, evaluation has relied upon stress testing, a more than 50-year-old technique designed to detect ischemia, an indirect sign that an individual has severe plaque buildup that narrows the artery and limits blood flow within it.
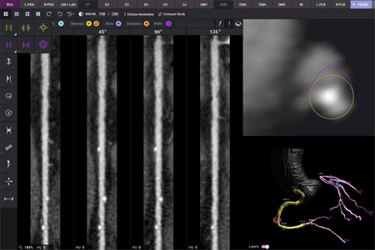
In contrast to risk factors and stress tests, coronary CT angiography (CCTA) is a novel non-invasive test that uniquely allows for direct visualization of atherosclerotic plaque. Large-scale clinical trials have discovered that there are several different types of atherosclerosis — and that these plaque “phenotypes” allow for discrimination of higher and lower risk disease. Longitudinal disease tracking has shown that beneficial lifestyle changes and medications transform higher-risk plaques into lower-risk plaques, a finding that is associated with >40% reduction in heart attacks and death. In an array of clinical trials, this approach has been shown to effectively democratize care across all patient subgroups, as an individual’s atherosclerotic plaque findings were the most effective predictors of heart attacks. Atherosclerotic plaque can effectively guide therapeutic decision-making, and heart attack risk based upon plaque findings is largely uninformed by risk factors, race, and gender but rather by an individual’s actual heart disease.
Notably, the new 2021 American Heart Association and American College of Cardiology professional clinical practice guidelines now endorse CCTA as Level IA, a higher level of recommendation than any other diagnostic test, establishing CCTA as the first-line standard of care. For the first time, these practice guidelines recommend atherosclerosis imaging to inform heart attack risk and track disease to ensure therapeutic success. By enacting CCTA as the de facto standard of care — and leveraging it to expand a patient’s understanding of their individual risk — we can improve outcomes for all patients by identifying disease earlier and with personalized precision.
Democratizing Cardiovascular Medicine With Artificial Intelligence
With CCTA, atherosclerotic heart disease can be diagnosed at a stage when it is readily treatable and when heart attacks can be easily prevented. In this regard, CCTA is well situated as the cornerstone to personalizing heart care, with at least two criteria required to effectively prevent heart attacks without bias.

First, a safe, non-invasive tool must allow for comprehensive quantification and characterization of disease. Analogous to how a non-invasive mammogram can stage the presence, extent, and severity of breast cancer, CCTA can serve as an accurate and rapid tool for routine evaluation of a patient’s heart disease and heart attack risk. Staging and classification allow for personalized, custom-tailored treatments that are effective for the individual. With improved software solutions that leverage the latest-generation artificial intelligence (AI), we can augment physician performance to superhuman levels of heart disease diagnosis.
Second, while CCTA is a non-invasive way to view disease state of the heart, it alone isn't enough to get a clear, unbiased, quantified measure of disease. Instead, we must focus on a cloud-first approach in next-generation medical devices, leveraging the massive computing power at our fingertips to analyze CCTAs and quantify disease. With the nearly unlimited storage and huge GPU capability of the cloud at our fingertips, we can train deep learning AI models on entire clinical trial data sets (terabyte and petabyte scale of imagery and associated metadata) to drive rapid and precise analysis previously unheard of. The days of performing all calculation and analysis within an installed medical device located on-premises at a hospital are nearing an end with the omnipresent connection to secure, massive software-as-a-service (SaaS) offerings that crunch numbers at speeds and scale unachievable previously. A cloud-first, always connected approach to medical devices is the future, marrying the scale of SaaS with the usability of a device present with the patient.
By personalizing and standardizing care through comprehensive assessment of an individual’s heart, AI-enabled CCTA will encourage assessment of individuals in a manner that can reduce the bias in today’s care that often miss persons of a differing races, ethnicities, and genders.
A New Paradigm Of Heart Attack Prevention
A “bespoke” approach to heart attack prevention can be easily implemented through AI-enabled CCTA solutions that improve individualized diagnosis and prognostic risk stratification, well-informed medical therapy and lifestyle choices, and quantitative disease tracking to ensure therapeutic success. But it is critical to ensure that these next-generation AI solutions are developed with diversity, equity, and inclusion in mind and to make certain that the AI is developed and validated with equal representation.
Although this precision heart care approach powered by AI-enabled CCTA can deliver personalized results, this new paradigm of care must also be coupled with delivery of this complex data to all the stakeholders in the care pathway, treating clinicians, imaging physicians, and patients in a manner that empowers them with understanding and actionable insights. These resources will encourage informed, proactive decisions about heart health that can effectively eradicate heart attacks.
We are at a unique point in time in cardiology, where the nexus of rapid improvements in machine intelligence, exponentially improved understanding of coronary vascular biology, and highly effective treatment methods are converging to enable a truly personalized approach to heart attack prevention. As we shift to this urgently needed approach, we must directly address the biases of previous evaluation methods that underperform in underrepresented populations, and instead directly assess individuals in a truly unbiased, personalized fashion. In doing so, we can standardize heart disease care globally, addressing one patient at a time.
About The Author:
 James K. Min, MD is founder and CEO of Cleerly. He is a former professor of radiology and medicine at Weill Cornell Medical College and the director of the Dalio Institute of Cardiovascular Imaging (ICI) at NewYork-Presbyterian. He is a board-certified cardiologist with a clinical focus on cardiovascular disease prevention and cardiovascular imaging. Min received his B.A. from the University of Chicago, and his medical degree from Temple University Medical School. He completed his internship, residency, and cardiovascular medicine fellowship at the University of Chicago Hospitals.
James K. Min, MD is founder and CEO of Cleerly. He is a former professor of radiology and medicine at Weill Cornell Medical College and the director of the Dalio Institute of Cardiovascular Imaging (ICI) at NewYork-Presbyterian. He is a board-certified cardiologist with a clinical focus on cardiovascular disease prevention and cardiovascular imaging. Min received his B.A. from the University of Chicago, and his medical degree from Temple University Medical School. He completed his internship, residency, and cardiovascular medicine fellowship at the University of Chicago Hospitals.
