Maximizing Clinician Involvement For Improved Device Design
By Natalie Abts, Genentech
When considering human factors for medical devices and combination products, running a validation test with the device’s target end users (often clinicians) is universally understood as the primary requirement to meet FDA expectations. Additionally, because finalized guidance documents regarding incorporation of human factors into device design have been available for some time, most developers are familiar enough with regulatory expectations that they also have learned the value of user testing in the formative stages.
device’s target end users (often clinicians) is universally understood as the primary requirement to meet FDA expectations. Additionally, because finalized guidance documents regarding incorporation of human factors into device design have been available for some time, most developers are familiar enough with regulatory expectations that they also have learned the value of user testing in the formative stages.
However, these activities are too often the extent of clinician involvement in the device lifecycle. Though user testing during development is critical, the tendency to utilize end users only for formal usability testing fails to harness clinician expertise at other critical points. This not only applies to the earlier stages of device development, before user testing is conducted, but also to the post-market stages, after FDA approval.
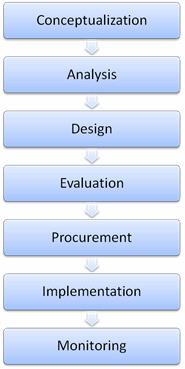
Fig. 1 — Example stages in the medical device lifecycle
Though the activities conducted during each phase of the medical device lifecycle are malleable, user involvement tends to be confined to the evaluation phase, and is less commonly seen in the earlier or later stages of the device lifecycle. The medical device industry has a shared responsibility among developers, healthcare systems, marketers, government, and other stakeholders to create devices that work well for clinicians so they can be operated with safety, efficiency, and satisfaction.
By restricting user involvement to a short window, we miss out on gathering data that can result in the production of devices that better achieve these goals. Two phases in particular, conceptualization and procurement, can perhaps benefit the most from additional clinician involvement.
Conceptualization
The concept development phase often is mission-critical to developing a device that works well for end users in the appropriate use contexts and use environments. Activities like market research, analysis of customer complaint data, and analysis of adverse events with similar products often are used to develop a new design, or to update the design of a predicate device. However, there are many potential advantages to expanding these activities to include end users in a more robust manner.
One reason to expand upon current concept research is that adverse event reporting is not likely to reflect all potential safety and usability issues, and may lack key details that give insight into design flaws. Near misses and close calls typically are not reflected in this data, and those types of events can be just as critical as serious safety events in the identification of device shortcomings. Thus, relying only on past reporting leaves serious gaps in the identification of areas for improvement.
Device developers may also rely on employees who are former clinicians to provide the majority of the end user input during conceptualization. These employees are sometimes out of clinical practice for a substantial amount of time, and may not be up to date on current practices. Relying on the opinions of one or two former users (particularly those who work for the developer) can introduce bias, and also may not reflect the varying experiences clinicians are expected to have across different healthcare environments.
Finally, common approaches in the conceptualization phase often lack a true systems perspective; that is, an approach to design that encompasses real-world device use that is not confined to a laboratory setting. Factors such as workload, physical characteristics of the use environment, operation in conjunction with other equipment, and time/space constraints all affect how a device is used once on the market. Thus, these system factors should be considered early in the development process.
One tool that is highly useful in gathering this type of data from clinical users is the ethnographic study (i.e., non-interfering observations in the clinical environment). This method allows observers to garner information on realistic use, rather than perceived ideal use. For example, while the intent may be for a device to be pole-mounted, the presence of a variety of other pole-mounted devices in the use environment may force users to keep devices on the floor, or to hang them on the bedside rail or footboard. Developers may want to consider how expected use is altered in these usage scenarios. This strategy may reveal system-level issues that may not be detected without direct observation of the end users.
Clinician users can be further involved in concept development via supplementary interviews and/or focus groups. When conducting ethnographic studies, it is important to allow users to perform their work in a realistic manner, without interruption from observers. However, post-observation follow-up discussions with clinicians can be even more revealing. You may find that users can provide further insight into observed behavior. For example, a clinician may be able to explain the purpose of workarounds, placement of devices, and interaction with predicate (legacy) products that were observed during the study.
Information gathered from clinicians can then be fed directly into other activities, such as evaluation of the legacy system. Positive and negative aspects of legacy devices (older models that the new product is intended to replace) can be both observed and discussed with the clinicians using them on a daily basis. Although market research activities can reveal some of this information, interviews conducted in a lab setting outside of the use environment are far less effective than discussions stemming from direct observation of device interactions.
Procurement
Taking advantage of clinician expertise is not just valuable for generating design inputs. Healthcare systems also should be utilizing their device end users to make smart procurement decisions. Many current procurement processes suffer not from failing to involve clinicians at all, but by involving them in a suboptimal manner. Input often is requested via subjective survey, with clinicians attending device fairs and sales demos to help them make a decision regarding device preferences. However, clinicians can provide far more value by participating in more formalized human factors activities.
Human factors engineers can utilize clinicians as data sources for a variety of usability activities that can be conducted during procurement, including feedback for legacy system evaluations and input on environmental constraints. However, the most useful way to involve clinicians is by engaging them in user testing. Although this is one of the most common ways to include end users during device development, it is utilized far less often as a procurement tool.
It may be difficult to understand why user testing should be necessary after a device already has been cleared by the FDA. Unfortunately, meeting the FDA’s human factors requirements does not guarantee the absence of safety and usability issues. Although a successful validation study is required for device approval, these studies only require evaluation with 15 users per distinct user group. While the majority of potential device problems can be detected with this number of users, some devices may have safety issues that occur infrequently and may not be detected during testing.
Another contributor to suboptimal device design is the FDA’s focus on usability issues specifically related to safety, rather than all usability issues. While it’s perfectly reasonable for safety to be the primary concern, this often means that companies trying to meet only the minimum requirements are not likely to make design updates to fix usability problems that are not safety-related. What we need to keep in mind is that these issues could still cause inefficiencies, frustrations, and workarounds. Because healthcare systems should be striving to obtain not only the safest devices, but also devices that work well for their end users, conducting independent usability testing with clinicians becomes critical to the decision process.
In a previous article, I described a case study of a healthcare system’s procurement of infusion pumps. In that example, a comparison usability study was conducted by human factors specialists to assess the safety and usability of two candidate devices for purchase. Although both devices were FDA approved, one was found to have several critical safety flaws. Additionally, usability issues unrelated to safety were discovered in both devices.
The value of the study, and the gathering of clinician performance data in addition to subjective information, is obvious from the hospital perspective. Not only did the results reveal a clear safety difference between the products, but the detection of non-critical usability problems in the safer device introduced the opportunity to prepare users to anticipate these issues, and to enhance training to promote knowledge of correct and efficient use.
Data gathered from clinicians during device procurement also has the advantage of serving multiple purposes. Not only can it be used to inform purchasing decisions, it can be a useful resource for future device redesign efforts. Developers can capitalize on these activities to generate solutions for any previously undetected usability issues, which can then be incorporated into next-generation devices. These studies also can encourage a more thorough application of human factors to design.
If more healthcare systems take steps to involve their clinician users in the procurement process via these robust methods, it could encourage developers to go beyond meeting the minimum usability standards acceptable for FDA approval. Developers will need to be more aware of addressing usability problems knowing that their devices will be compared to the competition using more extensive, user-centered data.
User input is a key component to designing any device, medical or otherwise, to fit with user needs. When use environments are as complex as healthcare systems, it is vital for clinicians to be involved at every stage of the product lifecycle. By utilizing the right methods at the right stages, the industry can produce more products that promote a safer, better work system for clinicians.
