Microneedle Patch Delivers Targeted Immunotherapy For Melanoma
Further studies of a microneedle-embedded drug delivery patch found that it provides a more robust response to immunotherapy cancer drugs than those administered using other methods to treat melanoma. In addition, researchers say the more targeted approach reduced the risk of side-effects inherent in immunotherapy treatments.
Scientists from two North Carolina universities — the University of North Carolina at Chapel Hill (UNC) and North Carolina State University (NCS) — first introduced the technology in a study published by ACS Nano last year. In it, engineers speculated the patch could be used to deliver a variety of drugs, including pain medication for arthritis patients, antibiotics for burn patients, and targeted therapy for cancer patients.
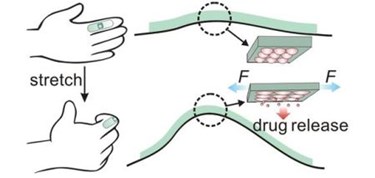
The patch is made from a biocompatible elastic film, covered with microcapsules containing nanoparticles preloaded with medications. The nanoparticles leak into the microcapsules over time, and when the patient moves and stretches the material, medication is released onto the skin, where it is absorbed. By adding microneedles to the original design, researchers found that they could deliver a transcutaneous dose of the drugs, as well.
More recent research published in Nano Letters found that the patch could provide an improved delivery method for immunotherapeutic drugs, a recent advance in precision cancer research. These therapies do not attack the cancer directly; rather, they block the mechanism by which cancers evade the body’s immune system.
According to researchers from Johns Hopkins, the surface of immune cells express a protein called programmed death-1 (PD-1) that teams up with proteins on cancerous cells to form a shield.
“Tumors can co-opt PD-1 to their own advantage to fly below the radar of the immune system,” said Suzanne Topalian, director of the melanoma program at Johns Hopkins. “By using a blocking agent against PD-1, we can interrupt that shield protecting the tumor from immune destruction.”
Chao Wang, co-lead author of the paper in Nano Letters and post-doctoral researcher at joint biomedical engineering program at UNC and NCS, explained that developments in anti-PD-1 drugs have presented challenges. First, an injection into the bloodstream is difficult to target, and second, an overdose of the drug can trigger an autoimmune disorder.
By using the patch, researchers found that a gradual delivery, over time, in a patch placed directly over the melanoma, provided a targeted response with a more controlled dosage, which reduced the risk of an auto-immune disorder, said Zhen Gu, senior author of the paper, in a press release.
In the study, researchers compared the patch with traditional injections of the drug, as well as injections directly into the melanoma in a mouse model. With the patch, they demonstrated a 40 percent survival rate, compared to zero percent from the other groups. Using anti-PD-1 in conjunction with anti-CTLA-4, the survival rate jumped to 70 percent.
Drug delivery by micro-needle patch is currently under investigation for a variety of indications. Scientists from the Centers for Disease Control (CDC) think a patch could be a “game-changer” for measles vaccination. Korean scientists recently introduced a microneedle patch integrated with graphene and gold that could be used to administer diabetes medication.
