Neuromodulation Dominates The U.S. Market For Neurological Devices
By Maryam Hashemi and Kamran Zamanian, Ph.D., iData Research

Neuromodulation devices are revolutionizing the treatment of neurological disorders by modulating nervous system activity through targeted electrical stimulation. These devices are used to manage conditions such as chronic pain, neurological disorders, epilepsy, urinary incontinence, and gastroparesis. These systems use electrical stimulation via implantable pulse generators (IPGs) connected to leads with electrodes targeting specific tissues.
Key neuromodulation types include spinal cord stimulation (SCS), deep brain stimulation (DBS), sacral nerve stimulation (SNS), vagus nerve stimulation (VNS), gastric electric stimulation (GES), dorsal root ganglion stimulation (DRG), and responsive neurostimulation (RNS). Emerging technologies like the BrainGate Neural Interface System are pushing the boundaries further, enabling individuals with motor impairments to control computers and potentially restore mobility through brain-machine interfaces.1,2
Market Review
The neuromodulation device market was the largest segment in the U.S. neurological device sector in 2024, as evident from the pie chart below. It occupies a significantly larger portion of the neurological device market than any other segments, making it the dominant area of investment and innovation. The widespread applications of neuromodulation in chronic pain management, movement disorders, and neurological conditions drive its prominence. In contrast, other markets, such as neurovascular thrombus management, neurovascular catheters, and stents, hold much smaller shares. While these segments are essential for neurological care, their market presence is overshadowed by the growing adoption of neuromodulation technologies. The chart clearly illustrates the increasing reliance on neuromodulation for treating neurological conditions, highlighting its leading role in this evolving industry.1
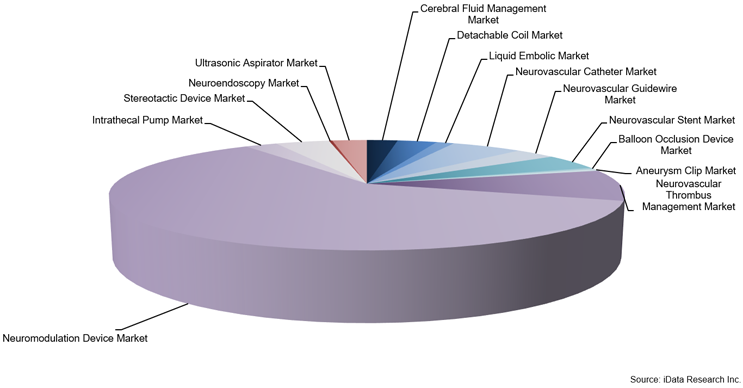
Figure 1: Neurological Device Market by Segment, U.S., 2024
The market for neuromodulation products is expected to grow considerably over the forecast period to reach over $5 billion by 2031. Market growth will be propelled by the wider acceptance of neuromodulation products, allowing them to be used in a larger proportion of potential patients. As new devices are developed and more indications are approved for this technology, the patient population will increase, driving unit sales. Additionally, neuromodulation products require replacement when their batteries become depleted, leading to continuing replacement sales. Many neuromodulation patients require multiple devices over their lifetimes because the battery life of neuromodulation devices is limited, ranging from three to 11 years, depending on the brand and patient usage.
Types of Neuromodulation Devices
Each neuromodulation approach offers unique therapeutic benefits for specific conditions:
- Spinal Cord Stimulation (SCS): SCS is a proven therapy for chronic neuropathic pain, including failed back surgery syndrome and complex regional pain syndrome. It involves implanting electrodes in the epidural space, connected to a pulse generator. Patients undergo a trial before permanent implantation. While traditional SCS operates at 40 Hz to 60 Hz, newer high-frequency and burst stimulation offer paresthesia-free relief. Advances in waveform technology and long-lasting rechargeable batteries are refining SCS for pain management and new applications like spinal cord injury recovery and Parkinson’s-related gait impairment.1,3
- Deep Brain Stimulation (DBS): DBS involves implanting brain electrodes linked to a pulse generator under the clavicle to regulate abnormal signals. Used for tremors and dystonia, its settings are wirelessly adjustable. Standard batteries last three to five years, while rechargeable ones exceed 15 years. DBS is a key therapy for neurological disorders, alongside cortical stimulation.1,3
- Sacral Nerve Stimulation (SNS): SNS devices treat urge incontinence, urinary retention, fecal incontinence, and urinary frequency by delivering electrical pulses to the sacral nerve, influencing bladder, sphincter, and pelvic floor function. The generator is implanted in the lower abdomen or buttock and offers a reversible treatment option. Patients undergo a trial period using a temporary electrode and external generator for three to five days, tracking their symptoms at home. If significant improvement is observed, a permanent implantable pulse generator (IPG) and lead are placed for long-term treatment.1
- Vagus Nerve Stimulation (VNS): VNS therapy has been an approved epilepsy treatment for over two decades, primarily for patients with refractory epilepsy who do not respond to medication. While antiepileptic drugs are the first-line treatment, VNS is recommended if they fail, with surgery as another option for some patients. VNS works by sending mild electrical stimulation through a lead to the left vagus nerve, helping regulate brain activity to reduce seizures. It is often used as an adjunct to medication for better seizure control.1
- Gastric Electric Stimulation (GES): Gastroparesis is a digestive disorder where food moves slowly through the stomach due to partial paralysis, often caused by conditions like diabetes, anorexia, and brain disorders. Symptoms include nausea, vomiting, bloating, and difficulty eating. GES is considered for those who do not respond to medications or cannot tolerate them. A GES system uses two leads with electrodes on the stomach wall and a neurostimulator in the abdomen to deliver mild electrical pulses to stimulate the stomach.1
- Dorsal Root Ganglion Stimulation: Complex regional pain syndrome (CRPS) is a chronic pain condition that often follows injury or surgery, typically affecting the limbs. While traditional SCS intercepts pain signals at the spine, a more targeted approach now stimulates the dorsal root ganglion (DRG), a key neurological structure involved in pain transmission. By delivering electrical pulses at around 200 Hz, DRG stimulation reduces abnormal nerve firing and blocks pain signals from reaching the brain. This therapy can be adjusted based on individual pain levels for more effective relief.1
- Responsive Neuromodulation: Epilepsy affects one in 26 people, with one-third having drug-resistant seizures. While surgery can control seizures, it is not always an option due to risks. Responsive neurostimulation (RNS) is an alternative, using a device that monitors brain activity and delivers electrical stimulation when abnormal patterns are detected. Unlike DBS and VNS, RNS operates in a closed-loop system, responding only to seizures. It reduces seizures by an average of 75%, but ongoing adjustments are needed for the best results.1,4
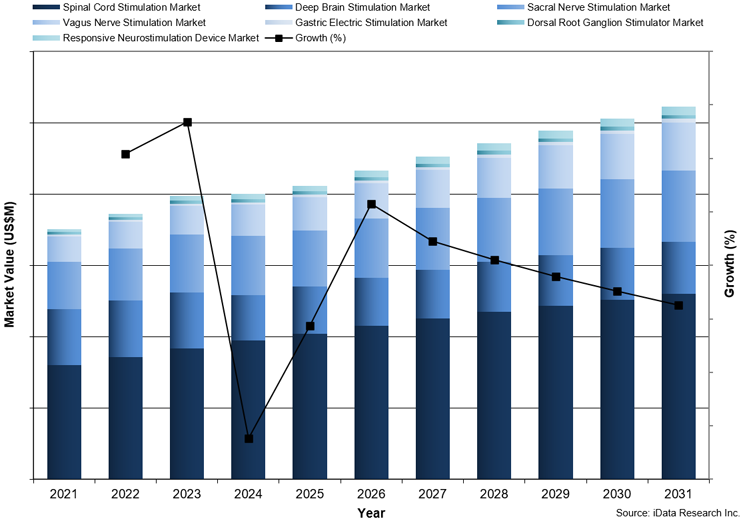
Figure 2: Neuromodulation Device Market by Segment, U.S, 2021–2031
The SCS segment was the largest in the neuromodulation market in 2024 and accounted for approximately half of the overall market value. This market is the most established neuromodulation market and is growing due to new product innovation. SNS is projected to become the second-largest segment by the end of the forecast period, with the DBS market becoming the third largest (Figure 2).1
Conclusion
Neuromodulation devices play a critical role in managing various neurological and pain-related conditions in the U.S. market, offering innovative treatment options beyond traditional pharmaceuticals and surgeries. With ongoing advancements in technology and expanding indications, the neuromodulation market is poised for significant growth in the coming years. As patient adoption increases and replacement cycles drive continued sales, the sector is expected to remain a dominant force in the neurological device industry. The widespread applications and evolving innovations underscore the importance of neuromodulation in shaping the future of neurological care in the United States.
References
- iData Research Inc. (2025). Global Urological Device Market. Vancouver
- International Neuromodulation Society. About Neuromodulation. Retrieved from neuromodulation.com: https://www.neuromodulation.com/about-neuromodulation
- B. Davidson, A. Battacharya et al. (2024). Neuromodulation techniques – From non-invasive brain stimulation to deep brain stimulation. Retrieved from Neurotherapeutics ELSEVIER: https://www.sciencedirect.com/science/article/pii/S1878747924000163
- V. R. Rao, J. D. Rolston. (2023). Unearthing the mechanism of responsive neurostimulation for epilepsy. Retrieved from Communication medicine: https://www.nature.com/articles/s43856-023-00401-x
About the Authors
Maryam Hashemi is a research analyst at iData Research. She develops and composes syndicated projects regarding the medical device industry, publishing the U.S. Peripheral Vascular Device Market report.
 Kamran Zamanian, Ph.D., is CEO and founding partner of iData Research. He has spent over 20 years working in the market research industry with a dedication to study of medical devices used in the health of patients all over the globe.
Kamran Zamanian, Ph.D., is CEO and founding partner of iData Research. He has spent over 20 years working in the market research industry with a dedication to study of medical devices used in the health of patients all over the globe.
