The Lasting Impact Of Telehealth On Dermatology May Only Be Skin Deep
By Natalya Stone, Susan Park, and Karina Ikeda

The COVID-19 pandemic changed how people engage with the healthcare system. Increased use of telehealth, for example, drove health systems and other providers to expand these capabilities and services, forcing behavioral changes from patients and physicians to adopt a largely unfamiliar form of care. Today, consumers and healthcare industry stakeholders have a desire to understand which aspects of virtual care should become a lasting element of patient-physician interactions.
Immunological diseases, which are often chronic and autoimmune in nature, received particular focus during the pandemic’s telehealth boom, due to COVID-19’s disproportional effect on immunocompromised patients. Teledermatology apps, which have been steadily rising in prevalence over the past five years,1 saw a sharp increase in use at the beginning of the pandemic as dermatologists virtually evaluated psoriasis, acne, and eczema patients to minimize COVID-19 exposure. For other specialists in the immunology space, including rheumatologists and gastroenterologists, telehealth became an effective tool to manage patients with chronic diseases, who require consistent follow-up.
Guidehouse undertook an analysis to understand the extent to which telehealth services in immunology persisted after the advent of COVID-19, and how, if at all, this varied across diseases.
Telehealth Claims Analysis
To track telehealth trends in immunology, key indications representing three broad therapeutic areas (rheumatology, gastroenterology, and dermatology) were selected for the analysis. Rheumatology included systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA), and gastroenterology included ulcerative colitis (UC). Dermatology included plaque psoriasis (PsO), atopic dermatitis (AD), chronic spontaneous urticaria (CSU), and hidradenitis suppurativa (HS). These indications were selected based on their widespread prevalence and chronic nature, requiring long-term disease management and regular follow-up visits with doctors.
TRUVEN Marketscan (2018–2021) data were used to analyze trends in commercial telehealth-eligible claims from 2018 through 2021 to cover pre-COVID-19, pre-vaccine COVID-19, and post-vaccine COVID-19 time periods. The average percentage of claims that were telehealth was determined for each indication at each time point.
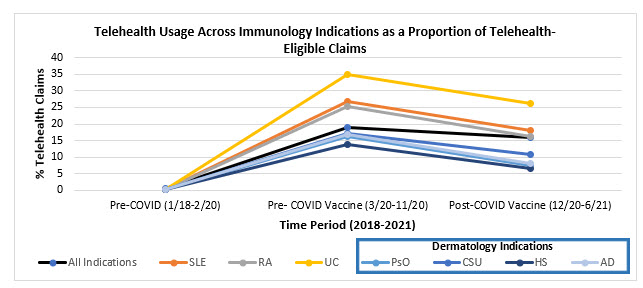
According to Guidehouse’s analysis, all four dermatological conditions stood out as consistently having the lowest average percentage of telehealth claims across all time points, compared to the indications in other therapeutic areas. This was an unexpected result, as dermatology is a therapeutic area that was predicted to have high levels of telehealth usage, due to advancements in teledermatology that allow greater accessibility of telehealth services for patients. The following hypotheses explore potential reasons for lower telehealth usage in dermatology indications during the COVID-19 pandemic.
Importance Of Visual Examinations
Lower observed usage of telehealth in dermatology compared to other indications could be attributed to the nature of dermatological indications. Dermatological conditions often require complete visual examinations by a physician to monitor and manage the skin. In contrast, other immunology indications can be monitored effectively through virtual appointments. For example, ulcerative colitis (UC) can be monitored by patient-reported gastrointestinal symptoms, which can be largely addressed through virtual appointments with occasional in-person checkups. The status of dermatological conditions like psoriasis are much more difficult to monitor with patient-reported symptoms alone.
Dermatologists note that although their primary form of care was via telehealth early in the COVID-19 pandemic, they are not convinced of the effectiveness of virtual appointments because of the difficulty in visualizing areas in question to provide adequate care.2 Additionally, the availability of personal protective equipment, protocols for screening, temperature checks, and mask requirements allowed dermatologists to resume in-person visits safely, reducing their need for telehealth.3 Although it has been found that patients prefer teledermatology over in-person visits due to long wait times for in-person appointments, physician skepticism regarding the effectiveness of virtual appointments, especially for complex dermatological conditions, may be a major driver of low telehealth use observed in this analysis.4
Lower Frequency Of Follow-up Appointments
Another potential reason behind the lower relative use of telehealth among dermatology conditions could be the general cadence of follow-up appointments for dermatology vs. other immunological conditions. Conditions such as SLE and UC tend to require more frequent follow-ups, roughly every three to four months,5,6 especially when patients are beginning a new treatment regimen and physicians need to monitor whether it is working for them. As such, it is feasible that these patients may be more inclined to conduct a portion of these follow-up visits virtually, especially if their treatment is adequately managing their disease.
In comparison, dermatology conditions typically require fewer follow-ups and are more likely to be seen on an as-needed basis. Psoriasis patients are seen one or two times per year7 once the condition is well controlled, and atopic dermatitis patients are seen only as necessary.8 Given this comparatively less frequent follow-up schedule, dermatology patients may be more inclined to see their doctor in-person.
Perceived Value Of Telehealth
The third possible reason for this observed trend in dermatology telehealth usage could be its lower perceived value compared to telehealth use in other more severe immunological indications. Rheumatologic conditions like RA and SLE are debilitating, painful diseases that cause fatigue and have a significant impact on patients’ daily activities and mobility. Therefore, the option of conducting a visit in the comfort of a patient’s home instead of traveling long distances to an office for an in-person visit might be highly attractive to patients who want to mitigate further pain and fatigue.
A 2021 study on the impact of telemedicine on management of RA found that the implementation of remote health monitoring at a rheumatology department in the Netherlands had a positive effect on health outcomes, including fewer hospital visits, compared to the total RA population.9 This finding could suggest that physicians treating RA patients recognized the positive impact of telehealth on their patients’ disease management and chose to optimize virtual appointments during the peak of COVID and afterward. A different 2021 study in Hong Kong on patients with SLE found that patients using telemedicine had a higher Physician Global Assessment score compared to patients receiving in-person care.10 The greater use of telehealth in SLE patients with higher severity also supports the hypothesis that there is a higher perceived value of telehealth in patients with debilitating immunological conditions.
While conditions such as HS and CSU can also be highly uncomfortable,11 much of the burdens of dermatologic conditions are perceived to be psychological and social rather than physically debilitating. An observational study of 151 dermatologists across centers in Spain found that while two-thirds of psoriasis patients in the sample had moderate to severe psoriasis, only 19.9% of overall patients had their quality of life routinely assessed by the dermatologists.12 Whether or not dermatologic conditions are equally as severe as rheumatologic conditions, there may be a perception that they have a less debilitating impact on quality of life and therefore less of a need for telehealth.
Implications For Future Patient Management
Despite the multitude of ways in which the COVID-19 pandemic brought about a sea change in the U.S. healthcare system, the Guidehouse analysis shows that telehealth within dermatology could not gain a substantial lasting foothold. As such, pharmaceutical manufacturers should not lose focus on the traditional and established ways physicians engage with patients in the practice environment and should continue to engage and support dermatology practices with this in mind. Given the unique considerations of dermatological conditions, including the importance of visual examination and other in-person interactions, it appears as if the traditional model of healthcare will remain, at least for the time being.
However, regardless of the factors that may currently be hindering the uptake of telehealth in dermatology vs. other immunological conditions, there is still a possibility of a hybrid environment moving forward. As teledermatology apps continue to evolve and patient preference is increasingly taken into consideration during shared decision-making, the care landscape could once again shift toward the virtual world, as it did during the peak of the pandemic. Pharmaceutical companies developing in the dermatology space should be poised to be agile, should these dynamics change, and keep watch on the newest technologies and telehealth capabilities to remain competitive.
References
- Flaten, H. K., St. Claire, C., Schlager, E., Dunnick, C. A., and Dellavalle, R. P., (2018), “Growth of mobile applications in dermatology - 2017 update,” Dermatology Online Journal, 24(2), doi: 10.5070/D3242038180.
- Kennedy J., Arey S., Hopkins Z., et al., “Dermatologist Perceptions of Teledermatology Implementation and Future Use After COVID-19: Demographics, Barriers, and Insights,” JAMA Dermatology, 2021; 157(5):595–597. doi:10.1001/jamadermatol.2021.0195.
- https://www.hmpgloballearningnetwork.com/site/thederm/article/how-does-telehealth-compare-traditional-person-visit-busy-dermatology-practice.
- Miller, J. and Jones, E., (2022), “Shaping the future of teledermatology: a literature review of patient and provider satisfaction with synchronous teledermatology during the COVID-19 pandemic,” Clinical and Experimental Dermatology, https://doi.org/10.1111/ced.15320.
- Gladman, D.D., Ibañez, D., Ruiz, I., Urowitz, M.B., “Recommendations for Frequency of Visits to Monitor Systemic Lupus Erythematosus in Asymptomatic Patients: Data from an Observational Cohort Study,” The Journal of Rheumatology, 2013, 40(5):630-633. doi: 10.3899/jrheum.121094.
- https://www.everydayhealth.com/ulcerative-colitis/symptoms/tackling-an-ulcerative-colitis-flare/#:~:text=During%20an%20ulcerative%20colitis%20flare,year%20to%20manage%20the%20
disease - https://www.webmd.com/skin-problems-and-treatments/psoriasis/find-psoriasis-doctor#:~:text=At%20first%2C%20your%20doctor%20may,go%20in%20every%206%20months
- https://www.webmd.com/skin-problems-and-treatments/eczema/remedies-for-eczema
- Müskens, W. D., Rongen-van Dartel, S., Vogel, C., Huis, A., Adang, E., & van Riel, P. (2021), “Telemedicine in the management of rheumatoid arthritis: maintaining disease control with less health-care utilization,” Rheumatology advances in practice, 5(1), rkaa079. doi: 10.1093/rap/rkaa079.
- So H., Chow E., Cheng I.T., Lau S-L., Li TK, Szeto C-C., and Tam L-S. (2021), “Factors Associated With Use of Telemedicine for Follow-Up of SLE in the COVID-19 Outbreak,” Frontiers in Medicine, 8:790652. doi:10.3389/fmed.2021.790652.
- Mian M., Silfvast-Kaiser A.S., Paek S.Y., Kivelevitch D., Menter A. (2019), “A Review of the Most Common Dermatologic Conditions and their Debilitating Psychosocial Impacts,” International Archives of Internal Medicine, 3:018. doi: 0.23937/2643-4466/1710018.
- Daudén, E., Conejo, J., and García-Calvo, C. (2011). Percepción del médico y paciente de la gravedad de la psoriasis, su impacto en la calidad de vida y satisfacción con la atención y el tratamiento recibido. Estudio observacional en España, [Physician and patient perception of disease severity, quality of life, and treatment satisfaction in psoriasis: an observational study in Spain]. Actas dermo-sifiliograficas, 102(4), 270–276. doi:10.1016/j.ad.2010.04.018.
Acknowledgments
We would like to thank Brian Kwak, a director in the Guidehouse Life Sciences practice, for his mentorship during the development of this piece.
 About The Authors:
About The Authors:
Karina Ikeda is a managing consultant within the Life Sciences practice at Guidehouse. She works across a wide variety of indications in immunology, and primarily focuses on opportunity assessments, product strategy, and patient support services. She holds a BA in public health studies from Johns Hopkins University, where her studies focused on health technology and policy.
 Natalya Stone is a senior consultant within the Life Sciences practice at Guidehouse. She works with pharmaceutical and medtech clients across a range of therapeutic areas, with a particular focus on market and product opportunity assessments and patient support services. She is heavily involved in the Guidehouse Immunology Expert Community and holds a BA in biological sciences from The University of Oxford.
Natalya Stone is a senior consultant within the Life Sciences practice at Guidehouse. She works with pharmaceutical and medtech clients across a range of therapeutic areas, with a particular focus on market and product opportunity assessments and patient support services. She is heavily involved in the Guidehouse Immunology Expert Community and holds a BA in biological sciences from The University of Oxford.
 Susan Park is a senior consultant within the Life Science practice at Guidehouse. She supports pharmaceutical and life science clients on a range of engagements, including market opportunity assessments, indication prioritization, global market access, and launch strategy. With nine years of experience as an immunologist prior to joining Guidehouse, Park has deep subject matter knowledge in various autoimmune and infectious diseases, which has contributed to successful engagements in commercial development. Susan received a Ph.D. in microbiology and immunology from Northwestern University and a BSc in biochemistry from UC San Diego.
Susan Park is a senior consultant within the Life Science practice at Guidehouse. She supports pharmaceutical and life science clients on a range of engagements, including market opportunity assessments, indication prioritization, global market access, and launch strategy. With nine years of experience as an immunologist prior to joining Guidehouse, Park has deep subject matter knowledge in various autoimmune and infectious diseases, which has contributed to successful engagements in commercial development. Susan received a Ph.D. in microbiology and immunology from Northwestern University and a BSc in biochemistry from UC San Diego.
