Unhealthy Healthcare Economics: Medtech Innovation As The Cure, Not The Cause
By Jim Pomager, Executive Editor
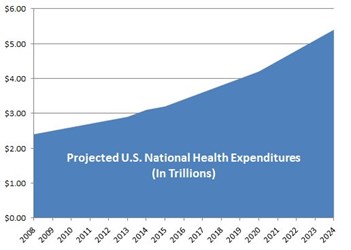
$3.2 trillion.
That’s about how much the United States will spend on healthcare in 2015, according to the Centers for Medicare and Medicaid Services (CMS).1 Yup, that’s trillions, with a “t”.
To put that figure in perspective, $3 trillion is more than the entire gross domestic product (GDP) of France. In fact, it’s greater than the GDP of all but a handful of the world’s largest economies.2 No matter how you slice it, the U.S. spends more on healthcare than any other country in the world — we have the highest total expenditure, the highest expenditure per capita (>$8,000), the highest percentage of GDP spent (17 percent), etc. And really, it’s not even close.3
One might assume that all this spending would translate to better health outcomes, but sadly, that is far from the case. Despite shelling out 2.5 times more on healthcare per capita than the average for member countries in Organisation for Economic Co-operation and Development (OECD), the U.S. has life expectancy rates that are one year lower than the OECD average.4 It’s obvious we have a major healthcare efficiency crisis on our hands.
A Demographic Headwind
Unfortunately, the situation grows more dire by the day. Even though Americans aren’t living as long as citizens in countries spending far less on healthcare, life expectancy in the U.S. has continued to inch up. As the massive Baby Boomer generation continues to age, it threatens to put additional strain on a healthcare system already stretched to its economic breaking point.
According to the U.S. Bureau of the Census, by the year 2040, over 20 percent of the population will be 65 years of age or older. By 2050, there will be nearly 90 million Americans in that age group — twice as many as in 2008. Between now and 2060, the number of people over the age of 85 will have tripled.5
U.S. Population Trends and Projections by Age, 1980 – 2060
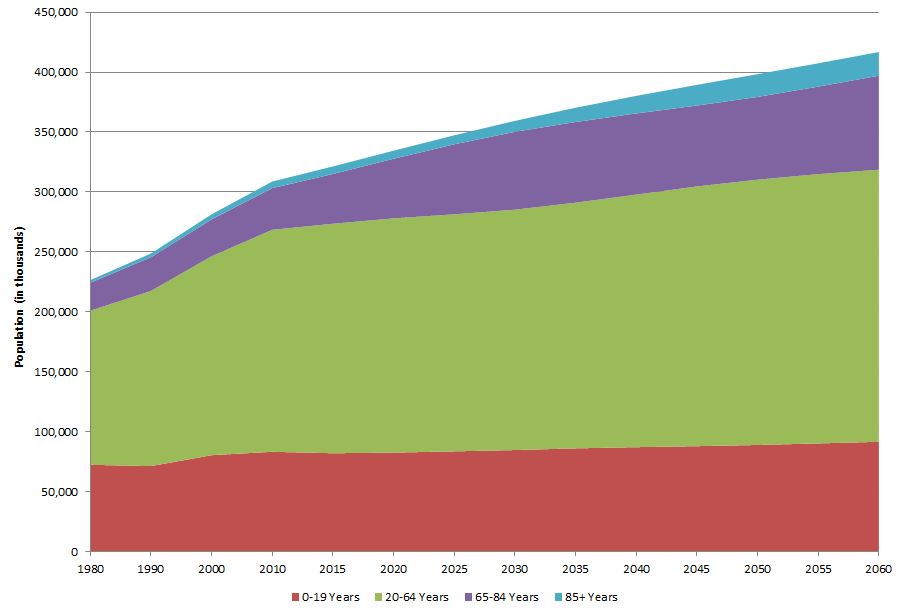
Source: U.S. Department of Commerce, Bureau of the Census. Projections of the Population by Sex and Age for the United States: 2015 -2060 (Years 2015 through 2060 are projections.)5
“We are running into a headwind of demographics,” Paul LaViolette, managing partner and COO of venture capital firm SV Life Sciences, said during the Medical Device Manufacturers Association (MDMA) Annual Meeting earlier this year. “We are not only seeing population increase in general, but we are seeing a skewing of our population toward the aged, and there will be far more folks on the Medicare enrollee list. Over the next 15 years, 10,000 new beneficiaries will be added to the Medicare rolls per day.”
LaViolette believes that this 65+ crowd — and more specifically, the chronic disease burden that they carry — is the root cause of the nation’s healthcare economy woes. Data published by the Centers for Medicare and Medicaid Services (CMS) shows that 69 percent of Medicare beneficiaries have two or more chronic conditions, and that those beneficiaries account for 93 percent of total Medicare spending.6 Patients with multiple chronic diseases consume the vast majority of U.S. healthcare resources, and this group is projected to grow by leaps and bounds in the coming years.
Distribution of Medicare FFS Beneficiaries by Number of Chronic Conditions and Total Medicare Spending, 2010
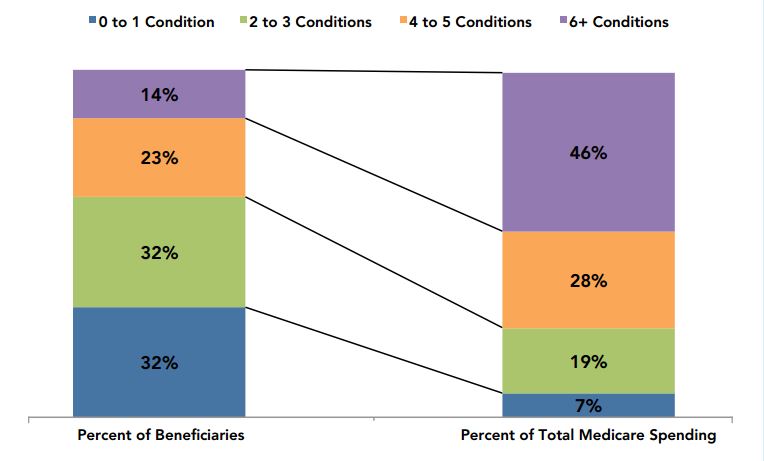
Source: Chronic Conditions among Medicare Beneficiaries — Chartbook: 2012 Edition6
“In less than 10 years, there will be an expectation of adding another trillion dollars to healthcare expenditure in the U.S. If this doesn’t convey a basic message that something has to change, I don’t know what does,” LaViolette added.
Aiming At The Wrong Target
I think everyone would agree that something does, indeed, need to change, and many have proposed solutions for how costs can be cut from the system. It’s too early to say whether systemic improvements like the Affordable Care Act (ACA) will be able to reverse the trend (in time), but while we wait around to find out, medical technology has become an all-too-easy mark for criticism and potential spending cuts, as those in the med device industry are well aware.
Case in point: robotic surgery equipment. Over the past few years, research groups have published numerous cost-effectiveness studies questioning the use of robotic technology in the operating room. They argue that surgical robots don’t deliver enough additional benefit or value over traditional laparoscopy to warrant their high price tags.
Imaging technology is another convenient scapegoat. A 2014 report (based on a survey of 192 hospital leaders) claimed that up to $12 billion is wasted on unnecessary imaging in the United States each year.7 Utilization rates may be higher than necessary, but that’s a system problem, not a technology problem, right?
“Nobody here wants to advocate unnecessary diagnostics or procedures. That’s not how we build sustainable franchises,” LaViolette told a room full of medtech executives. “My point is that those who criticize the industry often have small targets. They go after small stories, but in the larger scheme of the healthcare system, these medical device ‘problems’ pale in comparison.”
It’s true that the U.S. medical establishment sinks a lot of money into devices and diagnostics —north of $159 billion, to be exact (as of 2011, the latest year for which Census Bureau data is available). However, if you take a step back and a broader view of the situation, two things become clear. First, medical technology comprises a relatively small percentage (less than 6 percent) of the country’s total health spend. Second, it is an unusually stable component of the overall spend, hovering around 6 percent for the last two decades.
Medical Device Spending vs. National Health Accounts Expenditures, 1989-2011

Source: Estimates of Medical Device Spending in the United States, June 2014 8
Given these facts, surely there are more productive ways to curb spending than to single out medical devices. “We could spend not a future dime on medical technology, and it really wouldn’t change the overall cost of healthcare,” LaViolette said. “If you were the czar of the system for a day, this would not be the area where you would look to restrict spending, in order to make the system more effective. By all measures, expenditures on medical technology are very much in check.”
Developing Medical Devices That “Shift The Curve”
On the contrary, LaViolette argued that the way out of our current predicament is to devote more resources to medical technology, not less. By accelerating the development and integration of new med devices that target costly chronic diseases, we can take major steps toward lessening the chronic disease burden that currently threatens the system — and removing large chunks of cost from the national health economy.
“The healthcare spending curve is moving in the wrong direction, and the work we do may be one of the only hopes we have to shift that curve,” he said.
Take, for instance, heart failure, which is one of the most common causes of hospitalization in the United States. When you become a heart failure patient, your care is almost guaranteed to cost $100,000. There are currently over 5 million patients in the U.S. diagnosed with heart failure, responsible for a total of $32 billion in annual spending.9 Most of that spending, according to LaViolettte, goes to episodes of decompensation (restabilizing patients with acute heart failure) and disease maintenance (medications, routine doctor visits, etc.).
“Generally speaking, that means 95 percent of heart failure expenditure is not preventative in nature. It’s just pure maintenance of the status quo,” LaViolette pointed out. “Except it isn’t maintaining people. All acute heart failure patients are progressing, and 50 percent of them will die as a result of their heart failure within five years.”
“If we could come up with a therapy that reduced hospitalization rates associated with heart failure by only 5 percent, it would be worth $1 billion to the system. Maybe that’s something worth pursuing,” he added.
LaViolette pointed out two clinical-stage medical devices that could have a significant impact on heart failure outcomes and expense. One is CardioKinetix’ Parachute ventricular partitioning device*, which is designed to be implanted in the left ventricle of patients with systolic heart failure. The device isolates functional muscle from damaged muscle following a heart attack, allowing the heart to operate more efficiently. According to early clinical data coming out of a U.S. pivotal trial, the Parachute reduces mortality and hospitalization rates by somewhere between 30 and 50 percent.
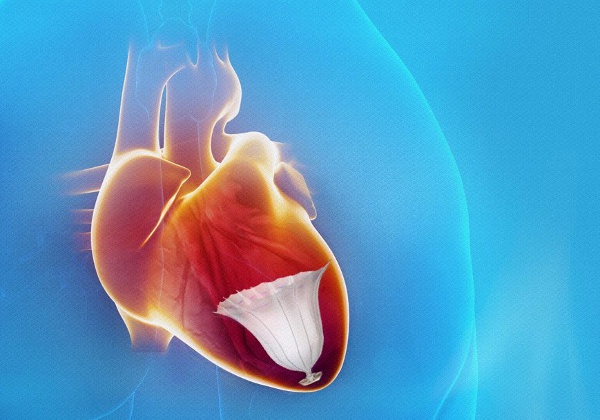
Source: CardioKinetix
Another heart failure-related example is the InterAtrial Shunt Device (IASD)* from Corvia Medical. This small, investigational device is designed to be implanted in the atrial wall, creating a very small opening between the left and right atria. The treatment is intended to reduce pressure on the left atrium and in the lungs, reducing symptoms and slowing the progression of diastolic heart failure. In clinical trials (outside the U.S.), the device has demonstrated a 67 percent reduction in heart failure hospitalizations.
“If a 5 percent reduction in hospitalizations is worth $1 billion, what would a 67 percent reduction be worth?” LaViolette asked.
Obesity is another chronic condition having a considerable effect on healthcare spending. It currently affects more than one-third of all Americans, and incidence levels are growing.10 Medical costs related to the condition amount to as much as $150 billion per year in the U.S., and each obesity patient consumes some $16,000 per year in healthcare resources. 11
Lifestyle modification (diet and exercise) and medical management are generally ineffective at treating the epidemic, as evidenced by its continued spread. Surgery, on the other hand, definitely works — and reduces costs — but remains an unpopular option. Only an estimated 0.3 percent of the total addressable obese patient population underwent surgical treatment in 2014.12
“Clearly, the marketplace is speaking that it does not want these major surgeries, even though they have a beneficial effect,” LaViolette said. “Technology has to have an effect in shifting the curve, because nothing else we’re doing today is capable of changing that curve.”
Obesity treatment is fertile ground for noninvasive technology alternatives. One example that LaViolette referenced was the ValenTx system*, a minimally invasive, adjustable, and removable device that allows food to bypass the stomach and duodenum, mimicking the mechanics of surgery but without the scalpels or staples. (The device is inserted into the stomach via the esophagus.) In clinical studies, the device resulted in a 45 percent reduction in excess weight and cardiovascular comorbidity resolution comparable to surgery.
“If you can get an obesity patient with a body mass index (BMI) of 42 down to 34, you will cut in half their expense burden on the healthcare system,” LaViolette explained. “And these are not patients that are 75 years old and getting an artificial heart; they are much younger, so helping them get reasonably healthy could have a 30-year impact on healthcare resource utilization.”
We Can Fix This
While the med devices described above could certainly help shift the curve of escalating health spending, they are only the tip of the iceberg. LaViolette mentioned that there is an “endless array of chronic opportunities” including:
- Glaucoma, the #1 cause of blindness in the U.S., where patients struggle with medication (eye drop) compliance
- Chronic obstructive pulmonary disease (COPD), which cost the U.S. approximately $50 billion in 2010 13
- Hypertension, on which nearly $43 billion is spent each year, with drug spending accounting for almost half ($20.4 billion)14
- Atrial fibrillation, which strikes 5 to 10 percent of those aged 65 to 85, and is responsible for about $24,000 in expenses per patient per year
- And the list goes on…
This is where you come in. Will you develop devices that make only incremental progress, or truly novel ones (like those described above) that will help shift the curve of runaway spending? Will you help dispel the accusations that medical devices and diagnostics add nothing but cost to an unhealthy healthcare system — by making data-supported economic arguments about your technology to payers, politicians, and naysayers? Will you be part of the multi-trillion-dollar problem, or part of its solution?
“When you look at the demographics underlying who we are, how long we are living, and how sick we are getting, you can actually get a little bit depressed about the prospect that the curve can possibly be shifted in the relatively near term,” LaViolette said. “But I would argue that the technology coming out of our companies is absolutely essential to solving the problem. We can fix this.”
* At the time of writing, all three of the specific devices referenced in this article are investigational, are not approved by the FDA, and are not available in the United States.
References:
- https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NationalHealthAccountsProjected.html
- https://en.wikipedia.org/wiki/List_of_countries_by_GDP_(nominal)
- http://www.who.int/mediacentre/factsheets/fs319/en/
- http://www.oecd.org/unitedstates/Health-at-a-Glance-2013-Press-Release-USA.pdf
- http://www.aha.org/research/reports/tw/chartbook/ch7.shtml
- https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Chronic-Conditions/Downloads/2012Chartbook.pdf
- http://research.peer60.com/unnecessary-imaging/
- http://advamed.org/res.download/684
- http://circ.ahajournals.org/content/123/8/933.long
- http://jama.jamanetwork.com/article.aspx?articleid=1832542
- http://content.healthaffairs.org/content/28/5/w822.full.pdf+html
- http://www.orthospinenews.com/wp-content/uploads/2014/10/researchnoteviewer.pdf
- http://www.chestnet.org/Guidelines-and-Resources/Health-Policy/~/media/49DEF1F46C62483F9C2B67232BB5377F.ashx
- http://meps.ahrq.gov/mepsweb/data_files/publications/st404/stat404.shtml
