Updated "Smart Insulin Patch" Uses Live Beta Cells To Produce Insulin
Researchers from the University of North Carolina (UNC) and North Carolina State (NCS) continue to develop a “smart insulin patch” that uses microneedles to detect rising levels of glucose in the bloodstream and then provides a dose of insulin if required. Previous patches were preloaded with synthetic insulin, but an update to the technology uses live beta cells instead, which researchers say reduces the risk of complication and lasts longer than the previous prototype.
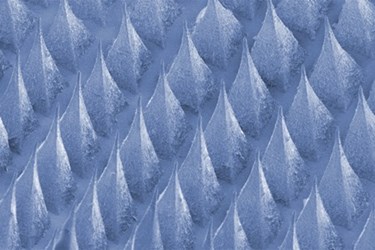
The biocompatible patch, introduced in a study published by Proceedings of the National Academy of Sciences (PNAS) last year, is roughly the size of a quarter and is embedded with microneedles the width of a human hair. Each of the needles is loaded with glucose-sensing enzymes and insulin, and if the enzymes sense a drop in the blood’s glucose, the insulin is released into the blood stream. The patch’s proof-of-concept study, using mouse models, found that it could regulate glucose levels for up to 9 hours, said the researchers in a press release.
According to Zhen Gu, a professor in the joint UNC/NCS department of bioengineering and co-senior author of the study, the system works quickly to correct glucose imbalances, is relatively simple to use, and is less painful than daily injections. John Buse, director of the UNC Diabetes Care Center, added that the patches can be customized to suit each patient’s individual needs.
“The whole system can be personalized to account for a diabetic’s weight and sensitivity to insulin,” said Buse, “so we could make the smart patch even smarter.”
In their latest advance, researchers have swapped out synthetic insulin for natural live beta cells — the part of the body responsible for producing insulin, and a study of the updated patch was recently published in Advanced Materials.
Diabetes is caused by damaged or underperforming beta cells, said researchers, but attempts to transplant healthy beta cells into diabetic patients are rarely successful, because the cells are rejected by the patient’s immune system.
“This study provides a potential solution for the tough problem of rejection, which has long plagued studies on pancreatic cell transplants for diabetes,” said Gu in a recent press release. “Plus it demonstrates that we can build a bridge between the physiological signals within the body and these therapeutic cells outside the body to keep glucose levels under control.”
In the updated system, beta cells are activated by “glucose-signal amplifiers,” which contain three chemicals to ensure that the cells respond to raised glucose levels. Because the beta cells remain outside the body, explained Gu, there is no risk of immune system rejection. Beta cell patches placed on mouse models regulated glucose for 10 hours.
Buse noted that the system is still in its preliminary stages and has not yet been tested on humans, and he told the Washington Post last year, “It will take years to work out whether this actually will work well in humans. But if it did, it would be amazing.”
