The Evolution Of Polymeric Materials In Vision Care & Ophthalmology
By Eric R. George, Ph.D., of ERG Polymers LLC

This is the third in a series of articles, the first titled An Introduction to Polymeric Materials for Medical Devices and the second, Polymeric Materials And Coronary Angioplasty Devices. These articles provide background information and context that aid the understanding of the current article.
“It is estimated that 1.3 billion people worldwide have some form of vision impairment (VI). Approximately 80% of VI is considered avoidable, with uncorrected refractive error being one of the leading causes. Refractive errors are broadly classified into myopia, hyperopia, astigmatism, and presbyopia, and may be corrected with the use of spectacles and contact lenses, or surgery.”1
Synthetic polymers play an essential role in spectacles, rigid gas permeable (RGP) and soft contact lenses (SCLs), corneal on-lays/in-lays, corneal scaffolds, intraocular lenses (IOLs), and vitreous humor replacement in vitrectomy. Biopolymers are critical in the structure and metabolism of the cornea, crystalline lens (lens), and the vitreous. “Modern polymer science and polymeric materials offer various alternatives, such as corneal and scleral implants, artificial ocular lenses, and vitreous substitutes, to replace the damaged parts of the eye. In addition to the use of polymers for medical treatment, polymeric contact lenses can provide not only vision correction, but they can also be used as wearable electronics.”2
Attributes of synthetic polymers for vision care applications include:
- Optical homogeneity and transparency (amorphous structures)
- High refractive indices
- Oxygen permeability
- Processability that is scalable and exhibits tight dimensional tolerances
- Biocompatibility
The Human Ocular System And Vision Science3
The key components of the eye for the purpose of this article are the cornea, lens, vitreous humor, and the retina (Figure 1). For the cornea, collagen, a polymeric protein, is the key structural component. The cornea is transparent, strong, and durable. It helps to shield the rest of the eye from harmful matter in synergism with the eyelids, the eye socket, tears, and sclera. Spectacles, contact lenses, and RGPs provide vision correction for vision defects in the cornea, lens, and overall length of the eye to restore proper focusing on the retina (the condition for good sight).4 The cornea accounts for over 60% of the focusing of light to the retina. The balance of focusing is largely attributed to the lens. Corneal irregularities and the changes of the overall eye length result in the need for spectacles, contact lenses, or LASIK surgery for the refractive error. Keratoconus (non-spherical corneal deformation) and astigmatism can be corrected via RGP. The aggregation of crystalline lens proteins with aging accounts for the stiffening of the lens (presbyopia) and the clouding of the lens (cataractogenesis). These conditions can be remedied with multifocal vision correction and cataract surgery (replacing the lens contents with an IOL), respectively.
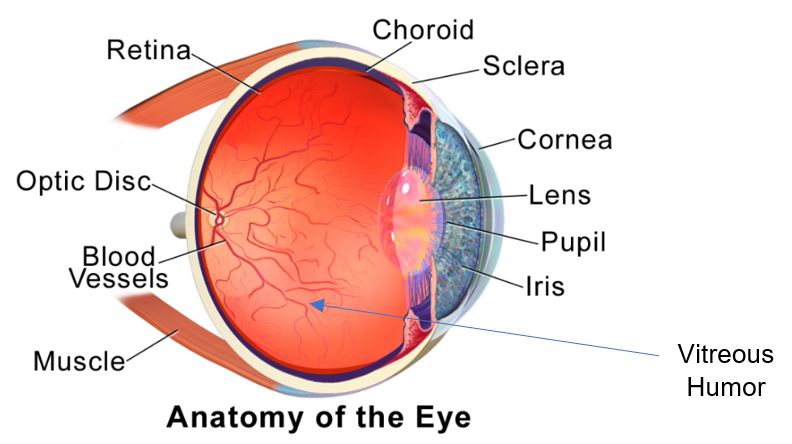
Figure 1. The Anatomy of the Eye. Courtesy of Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436. – This author’s own work.
The vitreous humor (VH) of the eye is composed of over 95% water and fibrillary collagen and the biopolymer hyaluronic acid (HA), where it was first discovered. This led to a whole host of HA applications, such as facial skin treatment and treatment of bone joints, for example.5 The VH is the largest segment of the eye and is critical to ocular homeostasis.
The retina is a multilayer structure that processes light by wavelength in the photoreceptors known as rods and cones. Most consider the retina to be part of the brain, as the light is processed and transferred to the brain (that serves as a biological CPU to generate images). Permanent vision loss in developed nations is predominately due to age-related macular degeneration (AMD). The macula is a small critical area of the retina for vision. In third-world countries, cataracts are the predominate cause of blindness as access to cataract surgery is not readily available.
Spectacles And Contact Lenses
For a thorough history of materials used in spectacles and contact lenses, please see reference 1.
In spectacles, product development led to polycarbonate (PC) lenses that are much lighter than glass, and modern PC lenses exhibit a high refractive index, are impact resistant, and have scratch resistant coatings and UV filters. PC progressive and bifocals are available to correct the VI of presbyopia.
For contact lenses, PMMA was the early material of choice for RGP but lacked oxygen permeability. This led to materials modified with silicones to provide oxygen permeability. These lenses can be uncomfortable, particularly in the early wear period.
Otto Wichterle and Drashoslav Lim developed soft contact lenses made of the hydrogel poly (2-hydroxyethyl methacrylate) (PHEMA). Later modification to increase water content by copolymerization with methacrylic acid led to biocompatible, comfortable SCL that remain a mainstay in the industry today. The addition of silicones (as done for RGP) to SCL led to higher oxygen permeability and extended-wear capability. Reference 6 is a representative academic study of how to modify the original HEMA-based polymers to yield improved oxygen permeability and other SCL attributes.
Current and future developments in contact lenses include orthokeratology (ortho-k) contact lenses for myopia progression (MP),7 photochromic contact lenses, combination SCL/API, and electronic enabled contact lenses. Myopia in children worsens with time and is an epidemic in Asian children. Spending time outdoors, tailored vision correction, and ortho-k slow MP. This is particularly relevant since children with MP are at higher risk for other ocular degenerative diseases. A photochromic SCL based on the Transitions® technology was recently introduced.8 In development are photochromic/antimicrobial SCLs for visual comfort and resistance to adverse events.9 Future electronic-enabled SCLs may provide better vision, help monitor and treat health conditions, and even deliver an interactive visual experience.10
The Crystalline Lens: Presbyopia, Cataract Surgery, And Prospective Treatments
The lens is a capsule (collagenous shell) filled predominately with a complex polymeric protein hydrogel composed of approximately 65% water and 35% proteins. These proteins aggregate with age, and beyond the age of about 43 the lens stiffens, resulting in the need for presbyopic vision correction (reading glasses). The proteins continue to aggregate, leading to cloudiness and the need for cataract surgery. In this surgery, the capsule is left in place and its proteinaceous contents removed with the aid of phacoemulsification then replaced with an IOL. Cataract surgery has made great progress since the first cataract surgery utilizing PMMA. Small laser-assisted incisions in the conjunctiva and capsule combined with foldable IOLs made of flexible silicones or other elastomeric polymers led to cataract surgery being one of the most successful surgeries, with well over a 99% success rate. Progress is constant to eliminate the predominate post-operative adverse event, posterior capsular opacification. 11,12
The aggregation of lens proteins is the fundamental pathway to presbyopia and cataracts. The three classes of polymeric structural proteins found in the lens are α, β, and γ crystallins. Major discoveries by Horowitz, Augusteyn, Truscott, and others that the α crystallins are chaperone proteins and are in finite supply was the foundation for prospective pharmaceutical solutions for interception and treatment.13,14
Several approaches are in development to intercept the progression of lens protein aggregation that expect to intercept presbyopia and cataractogenesis with topical solutions (eye drops).15-17
In the future, diagnostics will be critical to aid the implementation of these protein aggregation inhibitors. Dhadwal et al.18 developed a diagnostic based on dynamic laser light scattering that measures protein aggregation in vivo with age.
Vitrectomy (Vitreous Humor Replacement)19,20
Vitrectomy has become an important treatment option for ocular diseases, such as diabetic vitreous hemorrhage, retinal tear and detachment, uveitis, and ocular trauma. Liquid perfluorocarbons, sulfur hexafluoride gases, and saline buffers have been successful in vitrectomy for retinal detachments. Silicone oils are predominantly used for retinal detachments and are clinically accepted as a long-term vitreous replacement. Adverse events include elevation in intraocular pressure, retinal toxicity, and post-operative cataracts. There is a continuing search for long-term vitreous humor substitutes. Polymeric hydrogels are next-generation candidates in vitrectomy due to the ability to tailor their properties to closely mimic the natural vitreous. Thermosensitive smart hydrogels have emerged as a material class with great potential to succeed as ideal vitreous substitutes, facilitating easy implementation during surgery.
Conclusion
This article provides a cursory overview, with references, of the countless contributions to vision care by understanding and using polymeric materials. This is the quintessential display of the interdisciplinary research by polymer scientists, polymer physicists, chemists, engineers, optometrists, and ophthalmologists that has led to inventions, followed by commercialization of vision solutions. These outstanding achievements led to solutions for most visual impairments, but there remains work to provide these solutions to everyone globally.
In my forthcoming fourth and final article in the series, I will highlight the most profound impact of polymeric materials in medical devices and healthcare and include sections on controlled drug release, wearable sensors, and the future role of electrical and thermal conducting polymers.
References
- Rayishnee Pillay, Rekha Hansraj, Nishanee Rampersad, Historical Development, Applications and Advances in Materials Used in Spectacle Lenses and Contact Lenses, Clinical Optometry Vol. 12, p. 157–167, 2020.
- Metin Karayilan, Liane Clamen, and Matthew L. Becker, Polymeric Materials for Eye Surface, and Intraocular Applications, Biomacromolecules, Vol. 22, p. 223−261, 2021.
- Cassel, Gary H., Billig, Michael D., and Randall, Harry G., The Eye Book: The Complete Guide to Eye Disorders and Health, The Johns Hopkins University Press, 1998.
- The National Eye Institute https://www.nei.nih.gov/health/cornealdisease, Structures and Function of the Cornea, August 3, 2019.
- Craig A. Bettenhausen, Hyaluronic Acid, the Everywhere Biopolymer, C&E News, May 3, 2021.
- Nguyen-Phuong-Dung Tran and Ming-Chien Yang, Synthesis and Characterization of Silicone Contact Lenses Based on TRIS-DMA-NVP-HEMA Hydrogels, Polymers, Vol. 11, p. 944, 2019.
- FDA approves J&J Vision’s therapeutic contact lenses for myopia, Medical Device Network, May 13, 2021.
- J&J Vision Reports ‘Groundbreaking Contact Lens Using Transitions’ Technology, Vision Monday, Wednesday, April 11, 2018.
- Mengmeng Kang, Yaoyao Deng, Olayinka Oderinde, Fangfang Su, Wenjing Ma, Fang Yao, Guodong Fu, Zhihong Zhang. Sunlight-driven photochromic hydrogel based on silver bromide with antibacterial property and non-cytotoxicity. Chemical Engineering Journal 2019, 375, 121994.
- Melody M. Bomgardner, Making Better Contact Lenses, C&EN, p. 29, March 27, 2017.
- Manfred Tetz and & Matthew R. Jorgensen, New Hydrophobic IOL Materials and Understanding the Science of Glistenings, Current Eye Research, Vol. 40(10) p. 969–981, 2015.
- Mana Tehrania, H. Burkhard Dick, Beate Wolters, Tadeusz Pakula, Evan Wolf, Material Properties of Various Intraocular Lenses in an Experimental Study, Ophthalmologica, Vol. 218 p.57–63, 2004.
- R. J. Truscott, Presbyopia, Experimental Eye Research, Vol. 88 p. 241, 2009.
- Bron AJ, Vrensen GF, Koretz J, Maraini G, Harding JJ., The Aging Lens, Ophthalmologica, Vol. 214, p. 86, 2000.
- Gestwicki, Jason E.; McMenimen, Kathryn; Devree, Brian; Makley, Leah, Compounds and prodrugs of steroids and/or sterols for the treatment of ophthalmic disease such as cataracts that are inhibitors of α-crystallin aggregation, U.S. Pat. Appl. Publ., US 20200138832 A1, 2020.
- Muthukumar, Murugappan; Mohr, Benjamin, Methods of inhibiting cataracts and presbyopia, U.S. Pat. Appl. Publ., US 20160000707 A, 2016.
- Novartis to Acquire Encore Vision, Developer of Eye Drop for Treating Presbyopia, Vision Monday, December 16, 2016.
- Harbans S. Dhadwal and John Wittpenn, In vivo Dynamic Light Scattering Characterization of a Human Lens, Current Eye Research, Vol. 20(6), p. 502, 2000.
- Sruthi Santhanam, Ying-Bo Shui, Jessica Struckhoff, Bedia Begum Karakocak, Paul D. Hamilton, George J. Harocopos, and Nathan Ravi, Bioinspired Fibrillary Hydrogel with Controlled Swelling Behavior: Applicability as an Artificial Vitreous, ACS Appl. Bio Mater., Vol. 2, p. 70−80, 2019.
- Xinyi Su, Mein Jin Tan, Zibiao Li, Meihua Wong, Lakshminarayanan Rajamani, Gopal Lingam, and Xian Jun Loh, Recent Progress in Using Biomaterials as Vitreous Substitutes, Biomacromolecules, Vol. 16, p. 3093−3102, 2015.
About The Author:
 Eric R. George holds a Ph.D. in polymer science and engineering from the University of Massachusetts and a B.S. in polymer science from the University of Southern Mississippi. His expertise spans engineering thermoplastics, biodegradable polymers, biomedical devices, and diseases of the eye. He is currently with ERG Polymers, LLC, and has previously held positions at GE Plastics, Zeus Inc., and Johnson & Johnson (both Johnson & Johnson Vision and Janssen Pharmaceuticals). He holds 36 U.S. patents, has published 12 refereed journal articles, and is a certified Six Sigma Black Belt. He received the 2017 Outstanding Alumnus Award from the University of Southern Mississippi College of Science and Technology.
Eric R. George holds a Ph.D. in polymer science and engineering from the University of Massachusetts and a B.S. in polymer science from the University of Southern Mississippi. His expertise spans engineering thermoplastics, biodegradable polymers, biomedical devices, and diseases of the eye. He is currently with ERG Polymers, LLC, and has previously held positions at GE Plastics, Zeus Inc., and Johnson & Johnson (both Johnson & Johnson Vision and Janssen Pharmaceuticals). He holds 36 U.S. patents, has published 12 refereed journal articles, and is a certified Six Sigma Black Belt. He received the 2017 Outstanding Alumnus Award from the University of Southern Mississippi College of Science and Technology.
